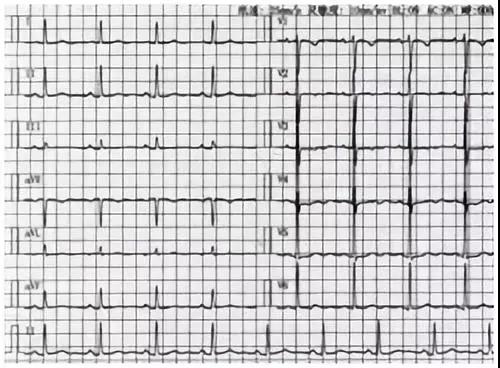
JAMA:P2Y12抑制剂单药治疗对PCI患者心血管事件的影响研究
2019-06-26 MedSci MedSci原创
研究发现,在接受经皮冠状动脉介入治疗的患者中,与延长DAPT方案相比,单用P2Y12抑制剂治疗3个月后患者主要不良心脑血管事件发生率无显著差异
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抑制剂#
29
#单药治疗#
29
#P2Y12#
41
#血管事件#
0
#PCI患者#
23
请问P2y12抑制剂用的是什么呢?
75
#2抑制剂#
24
#P2Y12抑制剂#
27
好好好好好好
64
学习了,谢谢分享
70