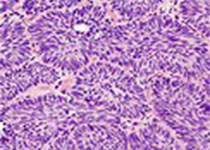
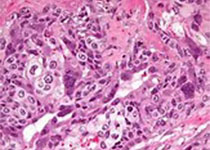
Blood:滤泡性淋巴瘤采用本达莫司汀联合利妥昔单抗治疗后早期病程进展提示高转化风险
2019-07-16 MedSci MedSci原创
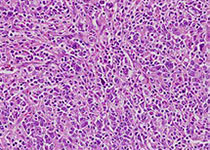
虽然本达莫司汀联合利妥昔单抗(BR)作为前线疗法广泛用于晚期滤泡性淋巴瘤(FL),但对早期进展或组织学转化的风险知之甚少。研究人员对296例以BR疗法+利妥昔单抗维持治疗的晚期FL患者进行回顾性分析。
本达莫司汀(bendamustine)联合利妥昔单抗(rituximab)作为前线疗法治疗晚期滤泡性淋巴瘤的疗效显著。
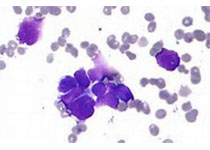
BR治疗后24个月内病程早期进展与预后不良相关,大多数患者会转化为淋巴瘤。
摘要:
虽然本达莫司汀联合利妥昔单抗(BR)作为前线疗法广泛用于晚期滤泡性淋巴瘤(FL),但对早期进展或组织学转化的风险知之甚少。研究人员对296例以BR疗法+利妥昔单抗维持治疗的晚期FL患者进行回顾性分析。
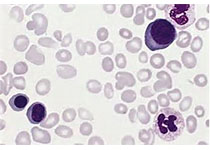
如前所述,这种方案的疗效很好,2年的无事件存活期(EFS)估计为85% (95% CI 80-89%), 2年的总体存活率(OS)为92% (95% CI 88-95%)。13%的患者在24个月内发生疾病进展(POD24),2年OS低于38% (95% CI 20-55%)。
基线时POD24唯一显著的危险因素是LDH升高。重要的是,大多数POD24患者(76%)已经发生病程转化。与既往接受RCVP治疗的队列相比,EFS有所改善,而POD24的风险有所降低,但发生POD24转化的患者比例更高。转化的总体发生率似乎没有变化。隐匿性或早期转化是前线BR治疗的FL患者POD24的主要驱动因素。
Ciara L. Freeman, et al. Early progression after BR is associated with high risk of transformation in advanced stage follicular lymphoma. Blood 2019 :blood.2019000258; doi: https://doi.org/10.1182/blood.2019000258
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#转化风险#
31
#利妥昔#
34
#滤泡性淋巴瘤#
35