Circulation:CRISPR/Cas9基因编辑或可用于治疗LDLR突变型家族性高胆固醇血症
2020-01-04 QQY MedSci原创
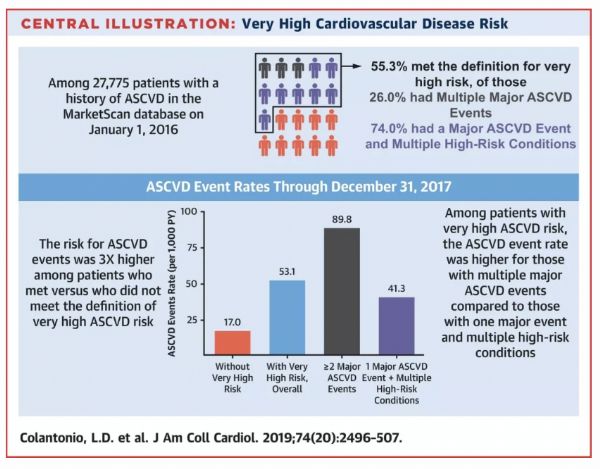
低密度脂蛋白(LDL)受体(LDLR)突变是家族性高胆固醇血症的主要原因之一,可诱发动脉粥样硬化,使携带者具有较高的终生心血管疾病风险。CRISPR/Cas9系统是基因编辑纠正基因突变从而改善疾病的有效工具。通过CRISPR/Cas9系统对体内体细胞进行基因编辑是否可治愈由Ldlr突变引起的家族性高胆固醇血症?本研究在小鼠模型中对此进行研究。研究人员基于相对应的家族性高胆固醇血症相关基因突变建立了
通过CRISPR/Cas9系统对体内体细胞进行基因编辑是否可治愈由Ldlr突变引起的家族性高胆固醇血症?本研究在小鼠模型中对此进行研究。研究人员基于相对应的家族性高胆固醇血症相关基因突变建立了一种无义点突变的鼠系——LdlrE208X。采用腺病毒(AAV)-CRISPR/Cas9校正肝细胞Ldlr基因上的点突变。
研究人员发现纯合突变的LdlrE208X小鼠(6只)经高脂膳食喂养后表现为严重的动脉粥样硬化表型,经AAV-CRISPR/Cas9治疗后部分肝细胞的Ldlr突变得到纠正,LDLR蛋白的表达部分恢复(6只)。与对照组相比(每组6只),靶向单导RNA的AAV-CRISPR/Cas9组(6只)的血清总胆固醇、总甘油三酯和低密度脂蛋白胆固醇均显著降低,而且主动脉粥样硬化斑块较小,巨噬细胞浸润程度较低。
本研究表明在体内用AAV-CRISPR/Cas9介导的Ldlr基因校正可部分恢复LDLR的表达,有效缓解Ldlr突变小鼠的动脉粥样硬化表型,为家族性高胆固醇血症患者提供了一种潜在的有效疗法。
原始出处:
Huan Zhao, et al.In Vivo AAV-CRISPR/Cas9–Mediated Gene Editing Ameliorates Atherosclerosis in Familial Hypercholesterolemia.
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#RISPR/Cas9#
44
#CRISPR/Cas9基因#
38
#LDLR#
32
#突变型#
33
#CRISPR#
33
#CRISPR/Cas9#
34
#Cas9#
41
#高胆固醇血症#
30
#LDL#
39
#Cas#
37