Int J Cardiol:年龄和性别对先天性心脏病成人存活率和死亡原因的影响!
2017-06-20 xing.T MedSci原创
由此可见,女性CHD患者的死亡率比男性要高。随着年龄的增长,CV死亡有所降低,但CV死亡的原因发生了重大的暂时性变化。在40以上的患者中,心脏衰竭超过猝死是幸存者的主要死亡原因。
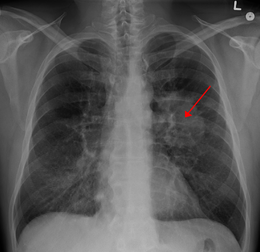
性别和年龄对成年先天性心脏病(ACHD)患者相对存活率和死亡原因的影响尚不明确。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员对3311例ACHD患者(50.5%为男性)进行了单中心观察性纵向研究,对其随访了25年。
研究人员根据参与者最后一次随访的年龄分为三组,分别为<40岁, 40-65岁和>65岁组。其生命状态是由西班牙国家死亡指数验证检查的。研究人员对参考人群的相对存活率进行回归分析。死亡原因是根据国际疾病分类代码(ICD-10)来进行分类。研究人员对因心血管原因死亡的病人进行个案调查。
累积随访时间为37608人次每年,死亡336例(10%)患者。女性年龄调整后的相对存活率明显低于男性(风险比为1.25;95%可信区间为1-1.6;P=0.046),三个年龄组的性别调整后的相对存活率有所提高(风险比为0.98;95%可信区间为0.97-0.99;p<0.001)。随着年龄的增长,男性和女性的心血管死亡均呈下降趋势(p<0.001)。导致心血管死亡的主要原因是心力衰竭,但在40岁以下的患者主要为猝死(P=0.004)。而随着年龄的增长,猝死率逐渐下降,心衰逐渐增多(p<0.001)。
由此可见,女性CHD患者的死亡率比男性要高。随着年龄的增长,CV死亡有所降低,但CV死亡的原因发生了重大的暂时性变化。在40以上的患者中,心脏衰竭超过猝死是幸存者的主要死亡原因。
原始出处:
Jose Maria Olivera,et al. Impact of age and sex on survival and causes of death in adults with congenital heart disease. International Journal of Cardiology. https://doi.org/10.1016/j.ijcard.2017.06.060
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#存活率#
23
#Cardiol#
30
#死亡原因#
31
#先天性#
26
非常好的文章,学习了,很受益
0
随着年龄增加,损耗增加
44
学习了,好文章谢谢分享。
54
学习了不少事情!
64
学习,谢谢分享
39