Mol Neurobiol:新的治疗方法或可有效对抗胶质母细胞瘤
2016-09-27 MedSci MedSci原创
胶质母细胞瘤是原发性恶性脑肿瘤最常见的形式。这些肿瘤具有高度增殖和浸润性,导致患者诊断后的中位生存期仅为14个月。目前的治疗方案对癌干细胞存在于肿瘤性微环境中的一小部分患者来说是无效的;然而,一种新的治疗方法或可在维持肿瘤干细胞表型的情况下将其移除至这种微环境的外面。 在体外研究人员已从人高级别胶质瘤(胶质瘤细胞球形成细胞(GSCs))中分离出多能成球细胞来研究这些细胞的粘附和迁移特性。由于
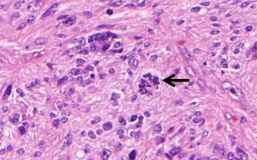
胶质母细胞瘤是原发性恶性脑肿瘤最常见的形式。这些肿瘤具有高度增殖和浸润性,导致患者诊断后的中位生存期仅为14个月。目前的治疗方案对癌干细胞存在于肿瘤性微环境中的一小部分患者来说是无效的;然而,一种新的治疗方法或可在维持肿瘤干细胞表型的情况下将其移除至这种微环境的外面。
在体外研究人员已从人高级别胶质瘤(胶质瘤细胞球形成细胞(GSCs))中分离出多能成球细胞来研究这些细胞的粘附和迁移特性。由于其在胶质母细胞瘤和GSCs中高度表达及激活细胞因子和生长因子的能力,研究人员重点专注了两个密切相关的基质金属蛋白酶ADAM10和ADAM17的作用。
结果发现,选择性抑制ADAM10和ADAM17 GSC的表达可增加GSC,但是并没有增加神经干细胞的增殖和迁移,且迁移的GSCs具有分化表型。
此外,研究人员还观察到Nestin,干/祖细胞标记物和纤连蛋白(一种在高级别胶质瘤组织中的表达的细胞外基质蛋白)之间存在关联。GSCs对纤维连接蛋白的粘附是由α5β1整合素介导的,纤维连接蛋白进一步促进GSC的迁移,且可促进体内肿瘤干细胞迁移出肿瘤性微环境。
总而言之,该研究结果表明,针对ADAM10和ADAM17的治疗或可促进癌干细胞迁移并远离肿瘤微环境,由此可使得肿瘤细胞分化为更容易治疗的表型.
原始出处:
Elodie J. Siney. Et al., Metalloproteinases ADAM10 and ADAM17 Mediate Migration and Differentiation in Glioblastoma Sphere-Forming Cells. Mol Neurobiol. 19 August 2016. DOI: 10.1007/s12035-016-0053-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胶质母细胞#
39
#Bio#
26
#Biol#
34
#母细胞瘤#
29
应该学习,继续研究
57
#治疗方法#
30
#细胞瘤#
27
这是一种全新的方法
58
好难,继续继续
68
:新的治疗方法或可有效对抗胶质母细胞瘤
61