Nat Rev Cancer:抗癌药研发新平台——类器官
2018-05-30 佚名 药明康德
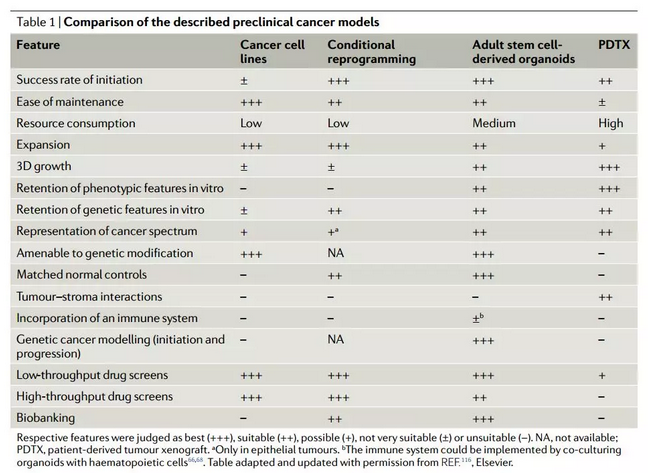
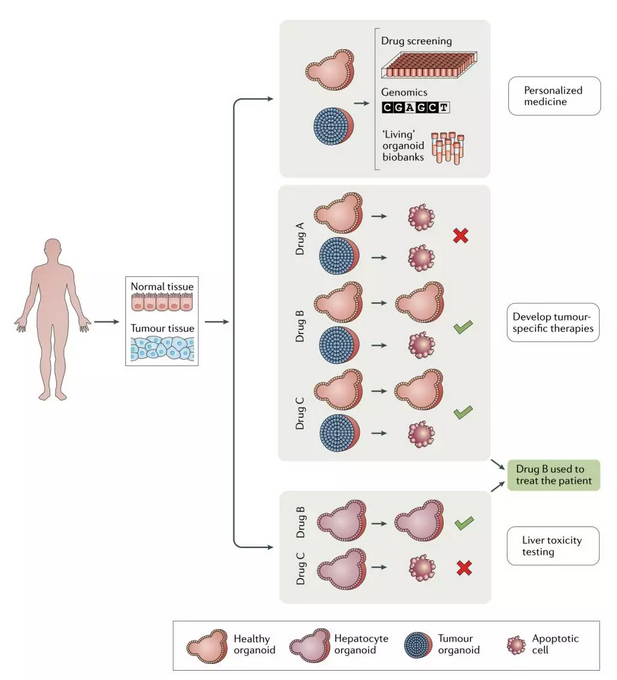
过去几年里,“类器官”(organoids)这个名词开始逐渐兴起,相信许多读者也都听说过它的名字。我们知道,类器官可以作为疾病模型协助新药研发,但它的具体应用,恐怕就不是每个人都能说清的了。近日,知名的《Nature Reviews Cancer》上发表了一篇综述,向我们介绍了类器官在癌症研发中的应用。在今天的这篇文章中,我们也将为各位读者整理其中的内容。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
41
#研发#
41
#抗癌药#
42
学习
84
谢谢分享.学习了
72
学习了.长知识
85
学习了
87