Cell:急性骨髓性白血病(AML)干细胞依赖昼夜节律环路的调控
2016-04-11 何嫱 生物通
一项新研究表明,昼夜节律环路对于急性骨髓性白血病干细胞(AML)而非健康血细胞至关重要,这为AML的治疗指出了可能的信号通路。 有一句俗话叫做“时间就是一切”。对于AML来说,这句格言可能是真的。在发表于4月7日《细胞》(Cell)杂志上的一篇论文中,由来自麻省理工学院与哈佛医学院Broad研究所、Brigham妇女医院(BWH)的研究人员领导的一个国际研究小组报告称,缺失它们的内部“钟表发
一项新研究表明,昼夜节律环路对于急性骨髓性白血病干细胞(AML)而非健康血细胞至关重要,这为AML的治疗指出了可能的信号通路。
有一句俗话叫做“时间就是一切”。对于AML来说,这句格言可能是真的。在发表于4月7日《细胞》(Cell)杂志上的一篇论文中,由来自麻省理工学院与哈佛医学院Broad研究所、Brigham妇女医院(BWH)的研究人员领导的一个国际研究小组报告称,缺失它们的内部“钟表发条”AML干细胞不能存活。
这些称作为昼夜节律的“发条”,充当了包括人类在内一些生物体的内部计时系统。昼夜节律可以根据大约24小时的日周期节律影响我们的睡眠/觉醒周期、代谢、激素生成和其他功能。这一周期的运转与环境条件如光线和温度相一致。
医学界很久以前就认识到了这些昼夜节律的存在。在过去的半个世纪,科学家们已经绘制出了一些维持这些发条运转的遗传回路。但还不清楚这一回路是否在每个细胞中都活化,或这种活性在癌细胞与健康细胞之间的差异程度。新研究发现昼夜节律回路在健康和癌性造血干细胞中均起作用。有意思地是,破坏这一回路(破坏“发条”的齿轮)会损害AML细胞的活力,而健康血细胞则未受损伤。
研究小组是在筛查白血病细胞生存必不可少的基因活性时获得这一研究发现的。
论文的资深作者、Broad研究所成员Benjamin Ebert,说:“Broad研究所Klarman细胞观测台的一项计划打算探究白血病干细胞的这一回路。我们与Broad研究所遗传干扰平台合作完成了一项遗传筛查,以鉴别出对AML干细胞旺盛生成必不可少的一组基因。”
令他们吃惊地是,在这些筛查中得分的两个基因是Clock和Bmal1——已知这些基因在一个复合物中协同作用调控了机体的昼夜节律。
论文的第一作者、Ebert实验室研究生Rishi Puram解释道:“在鉴别出Clock和Bmal1是我们遗传筛查的命中基因后,我们对此感兴趣的原因在于对于昼夜节律在白血病中的作用尚未有人进行过深入的研究。我们看到了一个发现某些新生物学的机会。”
在利用其他的方法(包括短发夹RNAs、CRISPR/Cas9和化学小分子)证实这些研究结果后,研究小组利用了一种只有血细胞内删除掉Bmal1 基因的“基因敲除”小鼠模型。该研究小组发现,尽管AML细胞需要Bmal1实现生长,正常造血干细胞在Bmal1不表达的条件下也可以存活。
“我们的研究表明,白血病细胞更依赖于昼夜节律回路:这两个基因表达对于白血病细胞的生存至关重要,而正常造血干细胞没有它也能存活。这正是我们在癌症生物学中寻找的——癌细胞与正常细胞的相对依赖性。这种依赖性可以成为一种治疗靶标,”Ebert说。
尽管研究人员强调还未确定是否可以利用这种依赖进行治疗,这些研究结果为未来的研究提供了诱人的可能性。
Puram说:“下一步是确定通过用一种药物直接扰乱这一信号通路,或通过在一天中AML细胞尤其易受伤害的时候按剂量给予化疗药物——这种方法叫做‘时间疗法’,来操控这一昼夜节律是否具有治疗作用。”时间疗法已在其他一些癌症类型,如胃肠癌和乳腺癌中显示出前景,但尚未证实对白血病有效。新研究结果提供了昼夜节律回路在AML中作用的一些重要见解,表明某一天时间疗法可作为AML或其他血癌患者一种有用的治疗方法。
Puram说:“鉴于我们的研究发现表明在AML中昼夜节律回路完好,白血病细胞中的这种基因表达在一天里周期性变化,这肯定值得去探索。我们是否能够利用它来实现治疗是我们一路向前有兴趣调查的一个问题。”
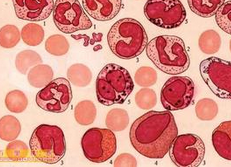
AML是一种骨髓性白细胞(而非淋巴性白细胞)异常增殖的血癌。其特点是骨髓内异常细胞的快速增殖而影响了正常血细胞的产生。AML是成年人最常见的急性白血病。
原始出处:
Puram RV, Kowalczyk MS, de Boer CG, Schneider RK, Miller PG, McConkey M, Tothova Z, Tejero H, Heckl D, Järås M, Chen MC, Li H, Tamayo A, Cowley GS, Rozenblatt-Rosen O, Al-Shahrour F, Regev A, Ebert BL. Core Circadian Clock Genes Regulate Leukemia Stem Cells in AML. Cell. 2016 Apr 7;165(2):303-316. doi: 10.1016/j.cell.2016.03.015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
35
PDF文件:http://sci-hub.cc/10.1016/j.cell.2016.03.015
143
请问 有人有PDF格式的吗
117
#CEL#
41
高大上的文章
127
值得学习
173
夜间效果好吧?
116
#急性骨髓性白血病#
36
#髓性#
22
学习了 长知识
74