综述:耳缺损修复的临床突破与挑战
2017-01-17 许枫,张如鸿,上海交通大学医学院附属第九人民医院整形外科 中国美容整形外科杂志
耳缺损是一种先天性和(或)继发性的耳郭畸形。其中,先天性耳郭缺失即先天性小耳畸形是整形外科常见病、多发病,在颅面部先天性畸形中,发病率仅次于唇腭裂。继发性耳郭缺失多为外伤所致,常见的原因包括咬伤、车祸、烧烫伤等。由于耳郭位于头面部,因此,耳郭缺损会对患者的容貌和心理产生巨大的负面影响。耳郭重建是目前治疗耳郭缺失的唯一途径,同时一直也是整形修复的难点。主要原因:首先,人类耳郭具有复杂的三维立体结
耳缺损是一种先天性和(或)继发性的耳郭畸形。其中,先天性耳郭缺失即先天性小耳畸形是整形外科常见病、多发病,在颅面部先天性畸形中,发病率仅次于唇腭裂。继发性耳郭缺失多为外伤所致,常见的原因包括咬伤、车祸、烧烫伤等。由于耳郭位于头面部,因此,耳郭缺损会对患者的容貌和心理产生巨大的负面影响。耳郭重建是目前治疗耳郭缺失的唯一途径,同时一直也是整形修复的难点。主要原因:首先,人类耳郭具有复杂的三维立体结构,体积较小,细节较多;其次,耳郭是由皮肤和软骨紧密贴合形成的复合组织器官,修复治疗需整合不同的组织,且组织来源有限。
自1959年Tanzer提出,并由Brent发展成熟的4期法全耳再造术以来,经过50多年的发展和改进,目前,全耳再造根据耳支架材料以及包裹耳支架的软组织来源不同,主要分为3大术式:(1)自体肋软骨2期再造法(nagata technique和上海九院法);(2)自体肋软骨乳突区骨膜上扩张法(park method)和单纯皮肤扩张法(北京整形外科医院法);(3)颞浅筋膜包裹Medpor支架I期全耳再造(JH Reinisch,2009年)。在实际的临床应用中,整形外科医师常常会发现再造一个外形逼真的耳郭是件非常困难的工作。常见的问题是,在实际操作中会有哪些细节影响了最终的手术效果?如何应用各种新技术更好地实施耳郭重建?未来还面临哪些问题与挑战?笔者将在下述内容中进行简要的评述。
1.肋软骨支架雕刻,由重建再造到美学再造
再造耳郭外形的逼真程度,基本上取决于耳支架的细节。人工材料(如Medpor支架)虽然可以通过计算机辅助制造出与健侧耳大小形态一致的效果,但由于人工材料的外露风险较大,自体肋软骨仍是耳郭再造的首选支架材料。因此,肋软骨支架的雕刻极其重要,除了要雕刻出合适的尺寸,还要复制足够多的细节结构。
在实施支架雕刻时,术者为了抵消皮瓣厚度的影响总是会夸大支架的细节结构,这种重建再造的理念对整形医师有着广泛的影响。然而,细节结构的过分夸张将导致再造耳郭结构浮雕化,给人以太假的感觉,导致患者及家属对再造耳郭不满意。其中,根据我们的调查,患者及家属抱怨最多的是再造的对耳轮及上下脚太高太假,不自然。为了解决这一问题,笔者尝试着对支架雕刻的细节进行改进。例如,临床观察提示,对耳轮复合体的形态对整个耳郭的自然呈现极为重要。
对耳轮复合体用底板残余软骨雕刻而成,同时在底板上挖槽,以实现对耳轮复合体与底板的自然过渡与衔接;在雕刻对耳轮上脚时避免出现高而窄的状况。对耳轮复合体通过不锈钢钢丝固定于底板。Y形复合体的添加不仅遮盖了6、7肋软骨联合处的切迹,还避免了对耳轮的台阶和不连续外观。这一改进使对耳轮、对耳轮上下脚、耳舟、三角窝、耳甲腔形态更加自然,进而使再造耳郭的整体形态逼真自然。
此外,雕刻支架时应特别注意各种细节,通常用6、7肋软骨雕刻底板,用第8肋软骨雕刻外耳轮及耳轮脚:底板的边缘应尽量薄而平滑,避免重建完成后,耳郭后面观呈厚重感。如第8肋软骨长度不足时,应注意通过拼接延长外耳轮,以避免术后呈外耳轮断裂感,因此,保持外耳轮完整的曲线是至关重要的;同时将一块V形软骨块固定于耳屏对耳屏复合体下,如果患者的软骨块充足,我们会增加一条软骨块,将其固定于耳轮脚底板与耳屏之间,将开放的半圆形耳支架固定形成闭合性结构,以避免支架长度和宽度的变化。
如果没有多余的软骨块,可用3-0编织线将耳屏及耳轮脚与基底固定以实现其稳定性。耳郭重建的发展过程大致可分为3个阶段:(1)1950~1980年。无法呈现足够多的解剖亚结构阶段;(2)1980~2010年。过度追求解剖结构的展现阶段;(3)2010年至今。自然的亚结构构建阶段。再造自然的耳郭亚结构是今后耳郭再造发展的方向。良好的重建结果不在于复制了多少亚结构,而在于复制了多少形态自然的亚结构,这是从重建再造到美学再造理念的转变。
2.数字化技术在耳郭重建中的应用
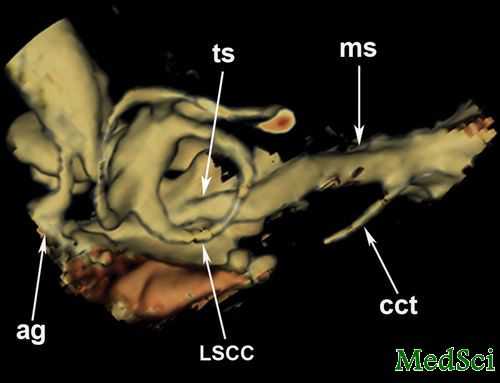
以计算机辅助设计为代表的数字化技术已广泛应用于整形外科的各个领域。数字化可以为耳郭重建提供客观可靠且有效的手术指导和术前设计。许枫等对拟行颅耳角重建的先天性小耳畸形患者。进行全头颅CT扫描,获取CT数据,同时在PC机上进行三维重建和设计,通过快速成形技术打印出实体模型,获得了个性化的骨水泥颅耳角支撑物,并应用于临床。
近1年来,3D打印技术在整形外科得到了快速地发展。梁久龙等在术前应用3D打印技术,打印出同侧肋软骨、镜像耳软骨及健侧耳的模型,术中应用此模型为患者雕刻个体化的耳支架,并在术后观察再造耳郭的形态,提高了再造耳与健侧耳的相似度。
3.赝复体在耳郭修复中的应用
在部分因严重烧伤、车祸外伤或头面部肿瘤切除导致的继发性耳郭缺损病例中,患者局部软组织损毁严重,颞浅筋膜血供受损甚至被切除,丧失了应用自体组织包裹耳支架修复耳郭畸形的条件,此时,选择义耳修复通常能获得满意的外观。大量的临床研究显示,应用钛种植体能获得良好的固位效果和美学重建,是目前义耳最佳的固位方式。
4.耳郭重建与听力治疗
先天性小耳畸形通常合并有外耳道畸形(闭锁或狭窄)、中耳畸形,并存在一定的听力障碍,主要表现为传导性听力损失。目前,耳科医师已达成共识:听力重建术(即外耳道成形及鼓室成形术)是一项极具挑战性的技术,必须慎之又慎。最近的文献报道,即在进行了严格的术前评估前提下,术后患者的听力改善并不理想,尤其是远期听力效果;另一方面,听力重建术后易发生外耳道狭窄、感染,甚至可导致面瘫和神经性耳聋等严重并发症发生。因此,对于单侧先天性小耳畸形患者,不主张行以耳道再通为主要手段的听力治疗;而对于双侧小耳畸形患者,如听力有严重损失的则成为治疗的难点。
通过近年来的科技发展和临床探索,目前这一难题有了比较合理的解决途径。植入式BAHA(骨锚式助听器)和振动声桥(VSB)在先天性小耳畸形伴耳道闭锁患者的听力治疗中获得了非常理想的效果,得到了耳科医师和整形外科医师的一致认可,很有可能会替代传统的显微外科听力重建术。
5.总结与展望
全耳再造是整形外科器官再造领域最具挑战性的工作,目前主流的3大术式均有各自较为明显的优缺点。总的来说,对于“自体肋软骨2期法”而言,肋软骨支架雕刻技术的不断改进是近年来临床治疗的主要突破点,但是,颅耳角的重建依然没有得到完美的解决;“乳突区皮瓣扩张法”则面临扩张皮瓣回缩不可控的问题;人工材料不耐磨,易外露,是Medpor支架在临床应用上最大的瓶颈;另一方面,再造耳郭与健耳位置的对称性也是影响术后效果的重要因素。对于合并有半侧颜面短小的先天性小耳畸形患者,通常会存在残耳耳垂位置过低、发际线偏低、乳突区凹陷等情况,使得再造耳的定位变得非常困难。
目前,这一问题还需进一步地探讨。技术的进步为耳郭的再造修复带来新的机遇。3D打印结合生物材料与干细胞技术将来有可能取代肋软骨成为新的耳支架材料;组织工程耳再造则已经开始实际的临床应用。我们期待未来耳郭的重建能获得更大的突破。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了,谢谢!
53
学习了,很好的内容
47
学习了,很好的内容
58
好文,值得点赞,值得拥有,值得收藏!
53
九院的技术不容置疑,但还是在排斥新方法
56
很不错
18
签到学习了…………
24
我们期待未来耳郭的重建能获得更大的突破。
29
3D打印结合生物材料与干细胞技术将来有可能取代肋软骨成为新的耳支架材料;组织工程耳再造则已经开始实际的临床应用。
25
大作拜读
27