Methods Mol Biol:优化的视网膜下注射技术用于基因治疗方法
2018-10-28 MedSci MedSci原创
德国EberhardKarlsUniversitat眼科研究所的MuhlfriedelR 等人近日在Methods Mol Biol发表了一篇文章,描述了一种新的方法,经巩膜睫状体进行载体病毒转移,为基因治疗提供新途径。
德国EberhardKarlsUniversitat眼科研究所的MuhlfriedelR 等人近日在Methods Mol Biol发表了一篇文章,描述了一种新的方法,经巩膜睫状体进行载体病毒转移,为基因治疗提供新途径。

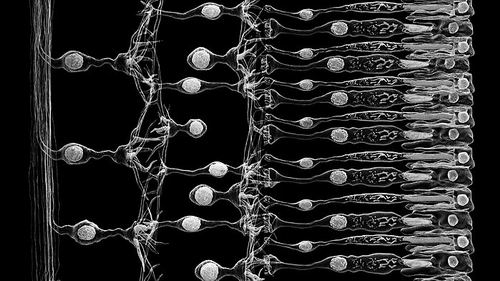
遗传性眼病的基因治疗需要通过眼内局部注射病毒载体。由于这些疾病大多数缺乏大型动物模型,因此,临床前验证研究大多用转基因小鼠模型。然而,由于小鼠眼睛相对较小,视网膜下递送过程本身不易进行,而这种不利影响可能会干扰治疗结果。
在这篇文章中,作者描述了一种新的方法,经巩膜睫状体进行载体病毒转移。在文章中,作者讨论了相关的细节,并对在小鼠眼中优化后的治疗效果进行了讨论。
原文出处:
Muhlfriedel, R., et al., Optimized Subretinal Injection Technique for Gene Therapy Approaches. Methods Mol Biol, 2019. 1834: p. 405-412.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MET#
49
#视网膜下注射#
31
#Bio#
30
#Biol#
36
#视网膜#
34
#治疗方法#
38
好
81
学习了,长知识
62
学习了
63