Blood:VWF的肝素结合结构域可结合生长因子促进新生血管形成
2019-04-13 MedSci MedSci原创
中心点:VWF的肝素结合结构域可与生长因子结合。在伤口愈合过程中,VWF的肝素结合结构域与生长因子协同促血管生成。摘要:在伤口愈合过程中,生长因子(GFs)通过结合创面微环境中的细胞外基质成分,调控其分布、有效性和信号传导。细胞外基质蛋白可通过结合GFs调节血管生成、促进伤口愈合。血管内皮细胞(ECs)在血浆和内皮下基质中释放的止血蛋白血管假性血友病因子(VWF)可调节血管生成;这种功能与VWF缺
VWF的肝素结合结构域可与生长因子结合。
在伤口愈合过程中,VWF的肝素结合结构域与生长因子协同促血管生成。
摘要:
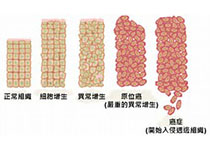
在伤口愈合过程中,生长因子(GFs)通过结合创面微环境中的细胞外基质成分,调控其分布、有效性和信号传导。细胞外基质蛋白可通过结合GFs调节血管生成、促进伤口愈合。
血管内皮细胞(ECs)在血浆和内皮下基质中释放的止血蛋白血管假性血友病因子(VWF)可调节血管生成;这种功能与VWF缺乏或功能障碍的患者的血管畸形相关。
Jun Ishihara等人发现小鼠VWF缺陷可导致伤口愈合延迟,同时伴随伤口中的血管形成减少、促血管形成的GFs减少。研究人员发现体外VWF与多种GFs结合,包括血管内皮生长因子(VEGF)-A亚型和血小板衍生的生长因子(PDGF)-BB,主要是通过VWF A1结构域中的肝素结合结构域(HBD)。在人类血浆中,VWF还可与VEGF-A和FGF-2结合;在EC中,VWF还可与VEGF-A共定位。
VWF A1-HBD与纤维蛋白基质结合后可隔离并缓慢释放结合的GFs。在VWF缺陷的小鼠体内,VWF A1-HBD功能化的纤维蛋白基质可增强血管形成和GF滞留。采用VEGF-A165和PDGF-BB联合VWF A1-HBD功能化的纤维蛋白基质治疗糖尿病小鼠的慢性皮肤损伤可加速伤口愈合、增加血管生成和平滑肌细胞增殖。
总而言之,VWF A1-HBD可作为GFs的储蓄池,促进有效的血管生成和组织再生。
Jun Ishihara, et al. The heparin binding domain of von Willebrand factor binds to growth factors and promotes angiogenesis in wound healing. Blood 2019 :blood.2019000510; doi: https://doi.org/10.1182/blood.2019000510
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#新生血管#
35
#肝素结合结构域#
30
#结构域#
39
#vWF#
33
#生长因子#
0