如何诊治感染性休克?看各类指南共识怎么说
2018-02-28 小艾 爱肝一生微课堂
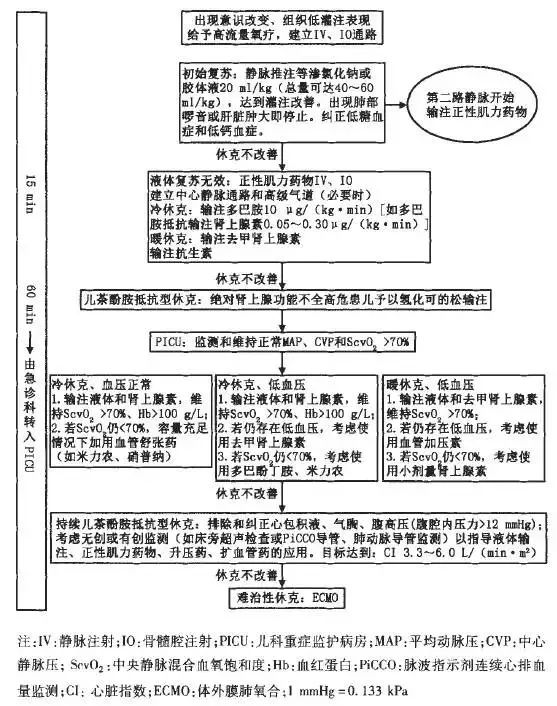
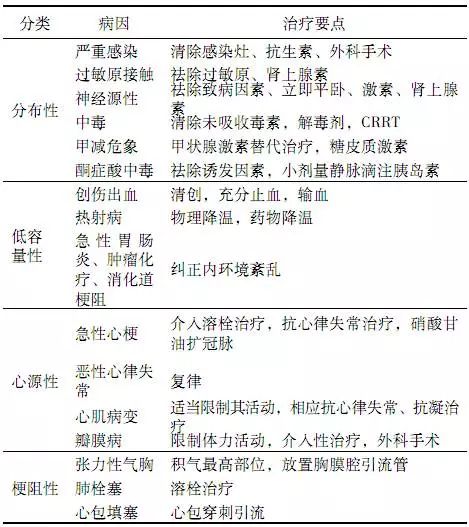
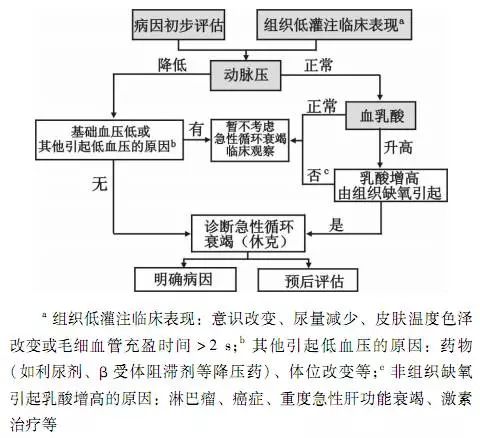
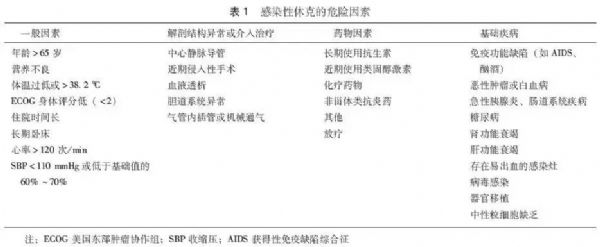
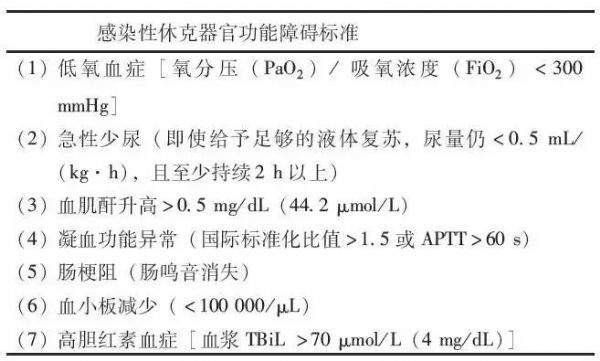
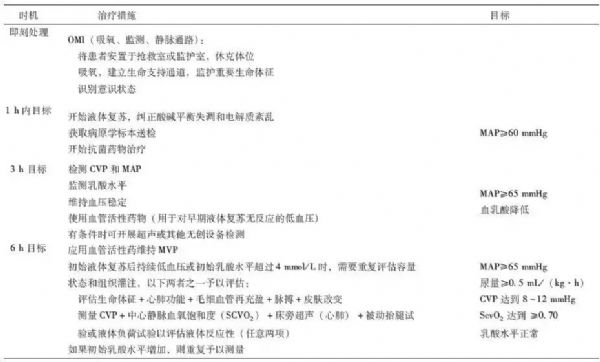
感染性休克(Septic Shock)是急诊科常见的急危重症,是指严重感染导致的低血压持续存在,经充分的液体复苏难以纠正的急性循环衰竭,可迅速导致严重组织器官功能损伤。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#感染性#
65
学习
74
很好.总结得很到位.学习了
67
学习
87
受教了.
84
学习.谢谢分享
73