Breast Cancer Res:乳腺X线密度与乳腺良性病变组织学特征相关性如何?
2018-01-02 曹守波 肿瘤资讯
乳房X线密度 (MBD) 反映了由乳房纤维腺体组织组成的乳房比例情况。临床工作中,约有40%以上接受乳腺筛查的女性会出现乳腺密度增高的现象。研究证实,MBD是乳腺癌 (breast cancer, BC) 发生公认的危险因素之一。相比于乳腺X线摄影非致密的患者,MBD最高水平的女性发生乳腺癌的风险要增加4-6倍。由于MBD升高可以掩盖致密组织内的肿瘤,因此也降低了癌症检出率的敏感性。
乳腺X线密度 (mammographic breast density, MBD) 升高已经被证实为乳腺癌发生的危险因素,并且可以掩盖致密组织内的肿瘤。然而,MBD与高风险良性乳腺疾病 (benign breast disease, BBD) 之间的关系尚不清楚。本文就这一问题进行了详细探讨,研究成果发表在《Breast Cancer Research》杂志。
乳房X线密度 (MBD) 反映了由乳房纤维腺体组织组成的乳房比例情况。临床工作中,约有40%以上接受乳腺筛查的女性会出现乳腺密度增高的现象。研究证实,MBD是乳腺癌 (breast cancer, BC) 发生公认的危险因素之一。相比于乳腺X线摄影非致密的患者,MBD最高水平的女性发生乳腺癌的风险要增加4-6倍。由于MBD升高可以掩盖致密组织内的肿瘤,因此也降低了癌症检出率的敏感性。
截至目前为止,MBD与高风险良性乳腺癌之间的关系尚未明确。了解致密乳腺组织中良性乳腺疾病的不同类型对于阐述MBD在癌变早期可能发挥的作用具有重要的意义,并且可以指导这一群体的筛查和诊断。本篇文献就致密和非致密良性乳腺疾病的组织学特征进行了系统性综合评估,并且探讨了致密乳腺疾病中乳房纤维化和小叶退化之间的差异性联系。
本研究共纳入了1985-2001年期间Mayo Clinic BBD队列中的3400名经病理证实的BBD女性患者,MBD的测量标准采用的是实质模式 (parenchymal pattern, PP) 或BI-RADS (Breast Imaging Reporting and Data Systems) 密度标准,具体分组标准如图1所示。入组的所有女性都进行了乳腺活检,经病理证实均显示与成像一致的良性结果。如果影像学和病理学结果不一致,则需要进行切除活检,如果活检结果提示恶性肿瘤,则患者被排除在研究之外。因此,本研究中并未纳入乳腺癌患者。所有乳腺活检样本均经过病理专家的组织学评价,危险因素的收集采用的是电子病历系统或电子问卷的方式。MBD被分为致密 (PP分类P2或DY,或BI-RADS分类c或d) 或非密度 (PP分类N1或P1或BI-RADS分类a或b)。
图1
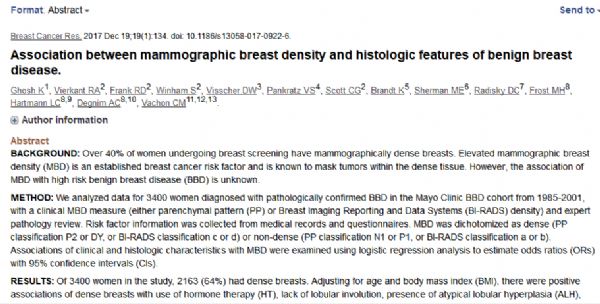
图2
病理学家评价良性乳腺病变的总体组织学分类包括非增殖性疾病 (non-proliferative disease, NP),非典型增生性疾病 (proliferative disease without atypia, PDWA)和非典型增生(包括非典型性导管增生,atypical ductal hyperplasia/ADH,或非典型小叶增生,atypical lobular hyperplasia/ALH)。此外,某些特殊的组织学特征包括柱状细胞增生 (columnar cell hyperplasia, CCH)、扁平上皮非典型增生 (flat epithelial atypia, FEA)、硬化性腺病 (sclerosing Adenosis, SA)、囊肿等也都被记录在内。由于CCH和FEA都代表了乳房组织中增生性柱状细胞的变化,因此将二者合并。根据切片中正常小叶的不同比例可以分为无退化(0%退化小叶),部分退化 (1-74%退化小叶)或完全退化 (≥75%退化小叶),详细可见图2。
3400例女性入组患者中,中位活检年龄为53岁 (小于40岁患者占13%,40-59岁占53%,60岁以上占34%),中位身体质量指数 (body mass index, BMI)为26,61%的患者既往或目前正在接受激素 (hormone therapy, HT) 治疗。在所有患者中,56%的女性患有非增殖性疾病,38%为PDWA,6%为AH。此外,64%的患者乳房密度较高 (60%采用BI-RADS“c”或“d”密度标准; 65%采用PP P2或DY标准)。
研究结果显示,发病年龄小、体重指数较低、既往应用过HT治疗以及活检时小叶退化程度较小与乳房密度增加明显相关。在调整年龄和BMI的模型中, ALH、纤维化、CCH/FEA、SA、囊肿,中到重度UDH以及钙化均与乳腺密度增高相关 (p<0.01)。而在调整多个变量后,年龄、BMI、HT、ALH、小叶退化、纤维化和CCH/FEA与乳腺密度增加显着相关 (p≤0.05)。纤维化可以使发生乳腺密度增加的几率升高2倍 (OR= 2.2, 95% CI= 1.9-2.6)。相比于小叶完全退化的患者,无小叶退化的患者发生乳腺密度增加的几率升高1.6倍 (OR= 1.6,95% CI= 1.2-2.1)。CCH/FEA同样与乳腺密度增加呈正相关 (OR= 1.3,95% CI= 1.0-1.7; p= 0.036)。诊断为ALH的女性相比于无ALH的女性,发生乳腺密度增高的几率升高50% (OR= 1.5, 95% CI= 1.2-2.1,p= 0.05)。
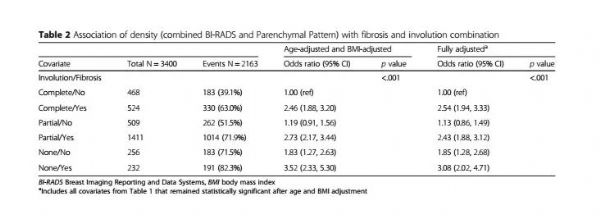
表2
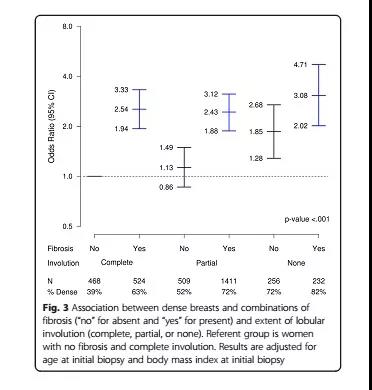
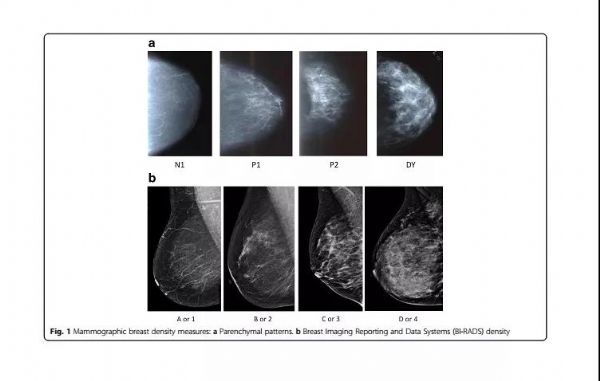
图3
表2和图3的结果显示了MBD与小叶退化和纤维化组合之间的联系。在调整年龄和BMI后的结果显示,相比于没有纤维化和小叶完全退化的女性,患有不完全小叶退化和/或纤维化的女性更容易发生MBD (p<0.05),其发生几率升高了3倍以上 (OR= 3.5,95% CI= 2.3-5.3)。在调整多变量分析后,尽管彼此之间的联系有所减弱,但是结果仍然显示高度的相关性。而进一步研究显示,小叶退化和纤维化之间并没有明显的相关性,结果无统计学意义 (在调整了年龄和BMI以及多变量模型中p值均大于0.2)。上述研究表明,小叶退化和纤维化对于发生MBD之间并无调节作用,二者都是单独对MBD产生影响。
患者是否经过HT治疗以及绝经前和绝经后与MBD发生之间的结果是相似的 (数据未显示)。当评价BI-RADS和PP标准的一部分女性与MBD发生之间的关系时,结果也是相似的。唯一的例外是,在BI-RADS评价标准下,囊肿的存在与非致密乳腺疾病的发生密切相关 (OR= 0.68, 95% CI= 0.47-0.97,P= 0.036),而这一结果在PP评价标准下并未得到证实 (OR= 1.17,95% CI= 0.81-1.68,p= 0.138)。
本研究对乳腺X线摄影中乳腺的密度与良性乳房组织的特殊组织学表现之间的关系进行了系统全面的评估。研究发现,在乳腺良性疾病的女性中,乳腺密度增高与纤维化和缺乏小叶退化有关。此外,与非致密乳腺的女性相比,乳腺密度增高的女性活检组织中发现ALH和CCH/FEA等高危病变的几率明显升高。
点评:本研究证实了MBD与纤维化以及缺乏小叶退化之间的关系。相比于乳腺X线摄影非致密的女性,乳腺密度增高的女性可能更容易罹患一些高危病变,如ALH和CCH/FEA,提示与MBD增高发生密切相关的高危因素可能会在乳腺癌发生的早期阶段扮演重要的作用。希望后续研究能够从乳腺致密组织中的乳腺上皮变化和分子标记物角度进一步阐明MBD,从而有针对性地降低乳腺癌的发生风险。
原始出处:
Ghosh K,et al.Association between mammographic breast density and histologic features of benign breast disease.Breast Cancer Res. 2017 Dec 19;19(1):134.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AST#
22
#组织学#
28
#相关性#
38
#X线#
27
#Breast#
27
学习一下知识了
63