JAHA:心肌纤维化标志物:揭示法布里心肌病纤维化的自然史!
2018-03-13 xing.T MedSci原创
由此可见,FD心肌病患者I型胶原合成增加,甚至在疾病的早期阶段,这种纤维化状态具有很好的预测价值,可能对于左心室肥厚的发生发展至关重要。此外,抑制I型胶原裂解的酶似乎对心肌胶原的沉积至关重要。
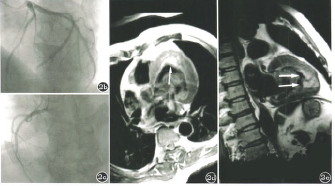
心肌病是影响法布里病(FD)预后的主要因素,心肌纤维化患者预后最差。晚期钆增强是目前评价心肌纤维化的金标准,然而,这一事件是不可逆的,因此识别早期弥漫性纤维化的生物标志物尤为重要。近日,心血管疾病领域权威杂志JAHA上针对这一主题发表了一篇研究文章。
研究人员评估了FD患者和对照者I型胶原的合成与降解的生物标志物(PICP[I型前胶原羧基端肽]、ICTP [羧基末端肽的I型胶原]和MMP1 [基质金属蛋白酶1]以及MMP2)和骨合成和降解标志物。根据超声心动图,将FD患者按心肌病严重程度分组:(1)正常,(2)组织多普勒异常,(3)左心室肥厚。
研究人员发现FD患者胶原基质金属蛋白酶显著降低,而PICP显著增加;即使在正常的超声心动图组PICP显著增加。研究人员还发现左室质量与PICP(ρ= 0.378,P=0.003)和MMP1(ρ=−0.484,P<0.001)之间存在显著的相关性。在多变量回归中PICP是左室质量更好的预测指标,其诊断准确性预测晚期钆增强也较为显著。
由此可见,FD心肌病患者I型胶原合成增加,甚至在疾病的早期阶段,这种纤维化状态具有很好的预测价值,可能对于左心室肥厚的发生发展至关重要。此外,抑制I型胶原裂解的酶似乎对心肌胶原的沉积至关重要。
原始出处:
Patrício Aguiar,et al. Biomarkers of Myocardial Fibrosis: Revealing the Natural History of Fibrogenesis in Fabry Disease Cardiomyopathy, JAHA.2018. https://doi.org/10.1161/JAHA.117.007124
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#自然史#
40
#标志物#
37
#肌纤维#
44
#AHA#
30
#肌病#
54