NEJM:常规PCI是选择生物可吸收支架还是金属支架?
2017-03-30 xing.T MedSci原创
这项在接受PCI患者中进行的试验的初步报告中,接受可吸收支架和金属支架的患者之间在靶血管衰竭的发生率上没有显著差异。通过2年的随访发现生物可吸收支架比金属支架出现支架内血栓的发生率较高。
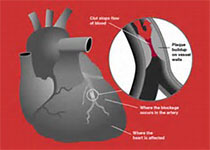
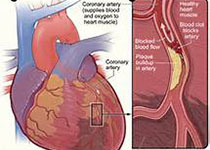
生物可吸收血管支架克服了药物洗脱支架在经皮冠状动脉介入治疗(PCI)中的缺点。最近,顶级医学期刊NEJM上发表了一篇研究文章,研究人员进行了一项在常规临床实践中比较依维莫司洗脱生物可吸收支架与依维莫司洗脱支架金属支架的随机试验。
研究人员将1845例接受PCI的患者随机分配接受生物可吸收血管支架(924例)或金属支架(921例)治疗。该研究的主要终点为靶血管失败率(心源性死亡、靶血管心肌梗死或靶血管血运重建)。数据和安全监测委员会建议提前报告研究结果,因为安全问题。该报告提供了关于终点事件的描述性信息。
中位随访时间为707天。在可吸收支架组发生靶血管衰竭的患者有105例,而金属支架组为94例(2年累积事件发生率分别为11.7%和10.7%;风险比为1.12;95%可信区间为0.85-1.48;P=0.43);事件发生率是基于时间事件分析中Kaplan-Meier估计。在可吸收支架组的患者中发生心脏性猝死的患者有18例,在金属支架组有23例(2年累积事件发生率分别为2%和2.7%),在可吸收支架组和金属支架组分别有48例患者和30例患者发生靶血管心肌梗死(2年累积事件发生率分别为5.5%和3.2%),可吸收支架组和金属支架组分别有76例和65例患者发生靶血管血运重建(2年累积事件发生率分别为8.7%和7.5%)。另外,可吸收支架组和金属支架组分别有31例患者和8例患者发生确定或可能的支架内血栓(2年累积事件发生率分别为3.5%和0.9%;危险比为3.87;95%可信区间为1.78-8.42,P<0.001)。
这项在接受PCI患者中进行的试验的初步报告中,接受可吸收支架和金属支架的患者之间在靶血管失败的发生率上没有显著差异。通过2年的随访发现生物可吸收支架比金属支架出现支架内血栓的发生率较高。
原始出处:
Joanna J. Wykrzykowska, et al. Bioresorbable Scaffolds versus Metallic Stents in Routine PCI. N Engl J Med 2017;http://www.nejm.org/doi/full/10.1056/NEJMoa1614954?query=featured_home
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#可吸收#
28
#生物可吸收#
33
#金属支架#
36
学习了
48
学习啦,谢谢分享
41