Int Arch Allergy Immunol:气道变应性炎症患者中,第二组先天性淋巴细胞的增加与嗜酸性粒细胞相关
2018-04-24 AlexYang MedSci原创
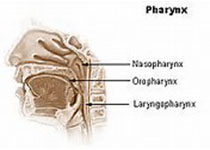
辅助T(Th2)类型响应被认为是过敏性气道疾病的本质,包括了哮喘和过敏性鼻炎(AR)。然而,有研究表明过敏性气道炎症同样依赖于先天免疫,并且与第二组先天性淋巴细胞(ILC2s)密切相关。最近,有研究人员在哮喘患者、哮喘和过敏性鼻炎患者以及健康个体中评估了ILC2的水平,并且尝试分析调查了临床数据和ILC2水平之间的关系。研究发现,哮喘患者和患有哮喘的过敏性鼻炎病人与健康对照相比,具有更低水平的IL
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了,谢谢作者分享!
71
#淋巴细胞#
27
#嗜酸性粒细胞#
39
#ALL#
32
#先天性#
28
不错的文章值得推荐
71
了解一下.谢谢分享!
74
不错的文章值得拥有
59