NEJM:高风险患者Bococizumab治疗的心血管功效和安全性如何?
2017-03-19 xing.T MedSci原创
在两项比较PCSK9抑制剂bococizumab和安慰剂的随机试验中,在主要不良心血管事件方面,较低风险的患者中bococizumab没有显著的获益,但在较高风险患者中bococizumab具有显著的临床益处。
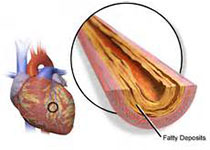
Bococizumab是一种人源化单克隆抗体,能够抑制前蛋白转化酶枯草溶菌素9(PCSK9)和降低低密度脂蛋白胆固醇(LDL)水平。近日,顶级医学期刊NEJM上发表了一篇研究文章。研究人员试图评价高心血管风险患者的bococizumab疗效。
在两个平行的、LDL胆固醇水平进入标准不同的跨国试验中,在这个联合试验中,研究人员随机分配27438名患者接受bococizumab(剂量为150 mg)或安慰剂皮下注射,每2周一次。该研究的主要终点为非致死性心肌梗死、非致死性卒中、不稳定心绞痛住院、需要紧急血运重建或心血管死亡,93%的患者在基线时接受他汀类药物治疗。试验因bococizumab产生抗药抗体且发生率较高赞助商选择终止bococizumab研发而过早停止试验。中位随访时间为10个月。
在治疗后14周,在联合试验中,接受bococizumab治疗的患者LDL胆固醇水平从基础水平平均下降-56%,而安慰剂组为2.9%,组间差异为-59个百分点(P<0.001)和从基线下降的中位数为64.2%(P<0.001)。在风险较低、持续时间较短的试验中(即患者基线LDL胆固醇水平≥70mg/dL [1.8mmol/L]和中位随访时间为7个月),在bococizumab组和安慰剂组发生主要心血管事件的患者为173例(风险比为0.99;95%可信区间[CI],为0.80-1.22;P=0.94)。在风险较高、持续时间较长的试验中(即患者基线LDL胆固醇水平≥100 mg/dL [2.6 mmol/L]和中位随访时间为12个月),发生主要心血管事件的患者分别有179例和224例(风险比为0.79,95% CI为0.65-0.97;P=0.02)。在联合试验中主要终点的风险比为0.88(95%CI为0.76-1.02;P=0.08)。注射部位反应更常见于bococizumab组相比于安慰剂组(10.4% vs. 1.3%,P<0.001)。
由此可见,在两项比较PCSK9抑制剂bococizumab和安慰剂的随机试验中,在主要不良心血管事件方面,较低风险的患者中bococizumab没有显著的获益,但在较高风险患者中bococizumab具有显著的临床益处。
原始出处:
Paul M Ridker, et al. Cardiovascular Efficacy and Safety of Bococizumab in High-Risk Patients. N Engl J Med 2017; http://www.nejm.org/doi/full/10.1056/NEJMoa1701488
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#高风险#
21
#mAb#
26
学习了,好文章。
35
签到学习了很多
33
学习了很多
45