心血管系统你一定要记住的5个关键英语词根
2019-02-13 MedSci MedSci原创
5个关键词根 01 cardi/o 心脏的 cardiology 心脏病学 cardiologist 心脏科专家 cardiovascular心血管 electrocardiogram心电图 cardiomegaly 心脏肥大 cardiomyopathy 心肌病 bradycardia 心动过缓 tachycardia 心动过速 cardiogenic
5个关键词根
01 cardi/o 心脏的
cardiology 心脏病学
cardiologist 心脏科专家
electrocardiogram心电图
cardiomegaly 心脏肥大
cardiomyopathy 心肌病
bradycardia 心动过缓
tachycardia 心动过速
cardiogenic shock 心源性休克
pericarditis 心包炎
endocarditis 心内膜炎
02 angi/o 血管的
angiogram 血管造影
angioplasty 血管成形术
angiotensin 血管紧张素 (ACEi认识吗?)
03 vas/o 血管的
vascular 血管的
vasoconstriction 血管收缩
vosodilation 血管扩张
04 atri/o 心房的
atrium 心房
atrial fibrillation 心房颤动
atrial flutter 心房扑动
atrioventricular 心房室的
05 ventricul/o 心室的
ventricule 心室
ventricular 心室的
interventricular 室间的
ventricular fibrillation 室颤
ventricular tachycardia 室速
延伸思考
心脏的冠脉解剖都能认得吗?

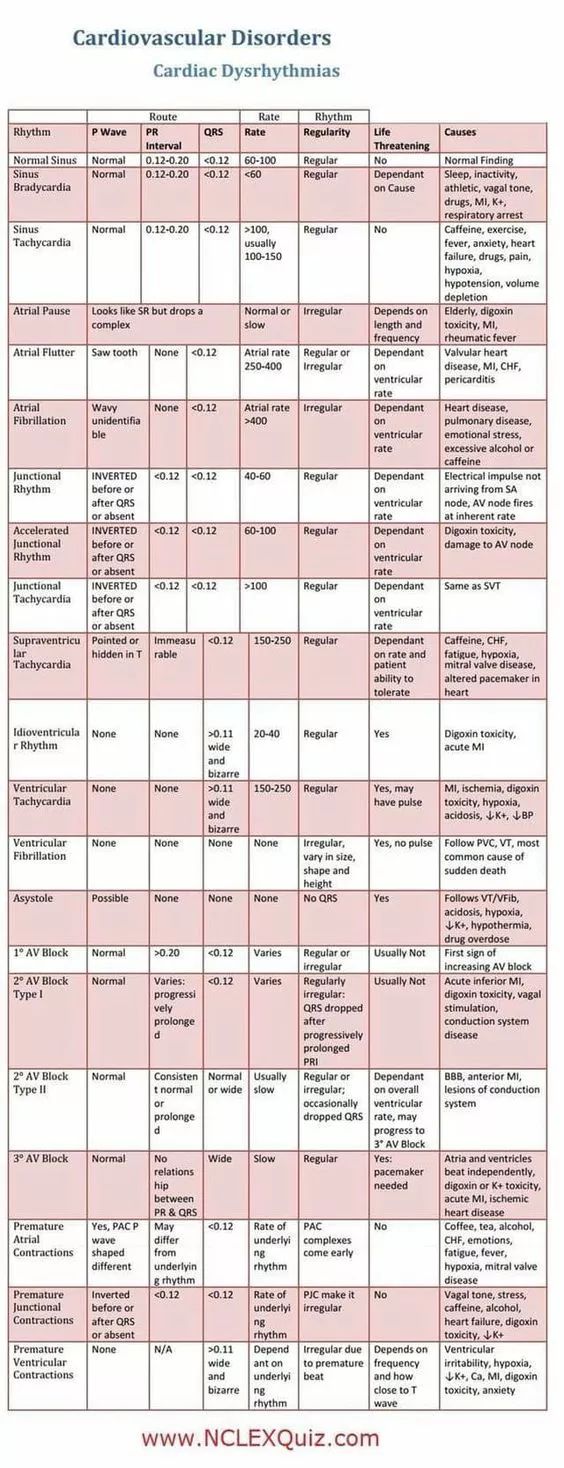
这些心律失常 (arrhythmia)
的词汇你都认识吗?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习#学习#
100
收藏起来!
0
cardi angi vas atri ventri
91
非常好👍
110
学习了,谢谢作者分享!
0