急性髓系白血病的“免疫治疗之路”已走了多远?
2017-12-02 佚名 中华全科医学
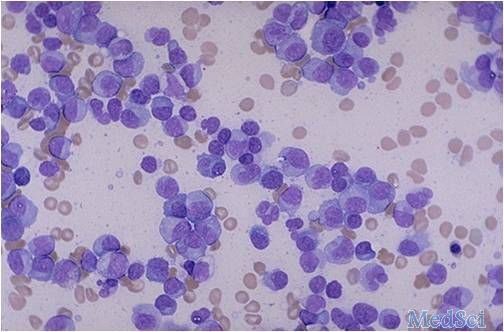
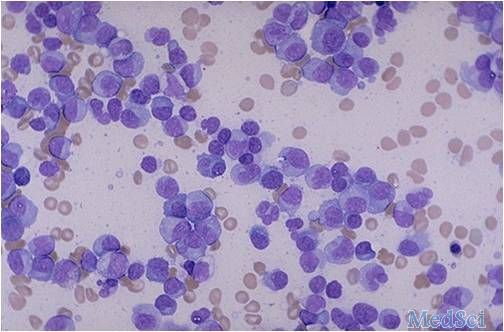
急性髓系白血病(AML)是不成熟的造血细胞在骨髓内聚集、不断扩增并抑制造血的一类疾病,其核心治疗方案近30年基本保持不变,但疾病的预后及生存率仍不理想。然而,目前针对机体免疫机制的研究使得免疫治疗得到不断完善,因此免疫治疗可能成为今后治疗AML的有效方案,为该病的预后及生存率提供了新的武器。本文将对目前AML免疫治疗的研究进展及相关分子学机制进行综述。 一、常规治疗方案 3
急性髓系白血病(AML)是不成熟的造血细胞在骨髓内聚集、不断扩增并抑制造血的一类疾病,其核心治疗方案近30年基本保持不变,但疾病的预后及生存率仍不理想。然而,目前针对机体免疫机制的研究使得免疫治疗得到不断完善,因此免疫治疗可能成为今后治疗AML的有效方案,为该病的预后及生存率提供了新的武器。本文将对目前AML免疫治疗的研究进展及相关分子学机制进行综述。
一、常规治疗方案
30多年前,“3+7”方案可使约60%的AML患者缓解,也因此成为治疗儿童和成人急性白血病的标准诱导治疗方案。上世纪90年代临床专家即开始关注缓解后治疗方案及其获益,并进行了大量的研究,其中包括高剂量阿糖胞苷化疗或造血干细胞移植(HSCT)。虽然儿童急性白血病的缓解率和总生存率现在分别大于90%和60%,但现有的治疗方案仍然基于蒽环类药物、核苷类似物及密集的缓解后治疗。为了提高AML患者的预后,临床也采用包括米托蒽醌与去甲氧柔红霉素的替代治疗、阿糖胞苷强化治疗等方案。然而大多数临床研究显示各治疗组的结局并不存在显著差异。尽管有这些令人失望的结果,但个体化治疗、支持性护理及造血干细胞移植将有助于提高治疗效果。
干细胞移植治疗白血病的疗效表明,抗肿瘤免疫可有效消除和防止白血病复发。事实上,许多研究表明,与化疗相比,造血干细胞移植的复发率明显降低。然而,由于造血干细胞移植具有很高的死亡率,因此在缓解期进行造血干细胞移植的适应证仍有争议。目前的情况显示,美国推荐的可适用HSCT的人群大于欧洲。
近年来,随着支持治疗的改进和更全面的HLA和NK分型有助于降低造血干细胞移植治疗的副作用。酪氨酸激酶抑制剂(TKIs)已成为目前重要的化疗方案之一。例如,FLT3基因(FLT3ITD)可引发约15%的儿童和30%的成人AML,且与不良结局相关,FLT3-ITD/野生型FLT3比例较高的个体表现更为显著。索拉非尼(sorafenib)、舒尼替尼和其他FLT3抑制剂可有效抑制FLT3突变,但长期使用这些药物则会出现耐药现象,这主要与D835或F691激酶区点突变引起有关。Crenolanib,新型酪氨酸激酶抑制剂,对于索拉非尼(Sorafenib)耐药的AML小鼠模型有较好的治疗作用,提示该剂可以延长临床受益。虽然TKIs提供了不同的白血病治疗方案,但仍处于发展阶段,临床需要更多的治疗策略。
二、单克隆抗体治疗方案
目前可用于治疗AML的潜在抗原包括CD33、CD123和CD47,其中CD33是研究人员集中关注的热点。2000年吉妥单抗奥左米星被用于治疗复发性AML。多项在成人及儿童新诊断白血病患者的临床随机试验提示儿童GO与常规化疗联合治疗可降低复发的风险,提高无事件生存率,并可能提高总生存期。Meta分析表明,复发风险低的患者是GO的最佳适应人群,中度复发风险人群获益较少,而高风险人群则无法通过GO治疗获益。
由于毒副作用和耐药性相关的局限性,研究人员已开发出一种新型的抗CD33抗体(SGN-CD33A)结合卡奇霉素。SGN-CD33A诱导治疗AML小鼠的疗效优于GO,目前正在进行Ⅰ期临床试验。为了提高CD33靶向治疗疗效,目前的方法是直接衔接的双特异性T细胞CD33/CD3(BiTE)抗体,如AMG330。其机制是将肿瘤抗原与T细胞受体(TCR)桥接,从而直接发挥T细胞杀伤肿瘤细胞的功能。动物研究表明,AMG330能够招募T细胞,从而有效发挥CD33依赖的细胞毒作用。类似于BiTE,NK细胞的双特异性杀伤抗体可靶向CD16。CD16xCD33特异性抗体及CD16xCD33xCD123抗体已经证明可诱导NK细胞发挥细胞毒作用,消除表达CD33的急性白血病细胞。
三、自然杀伤细胞治疗方案
自然杀伤(NK)细胞可以在未暴露过的情况下靶向杀灭白血病细胞。2002年首次有研究证实,杀伤抑制受体(KIR)与供体不匹配的NK细胞可通过异基因造血干细胞移植治疗AML,后来该结论被更多研究证实。随后,有研究人员发现,在AML患者体内输注NK细胞可减少免疫耐受并不会出现移植物抗宿主疾病。虽然这些结果提示结合NK细胞治疗可安全、有效降低AML复发风险,但仍需要更多的临床研究证实。此外,增强NK细胞活性可能是今后最佳的白血病治疗方案。
目前用来提NK细胞数量和活性的方案,包括扩增活化的NK细胞、RXR激动剂或γ谱系特异性抗体,如抗CD33。增强NK细胞杀伤活性的另一种方法是抗体阻断抑制性KIR,其可阻断KIRs,这种方法最近被证明在AML患者体内是安全的。调节性T细胞(Treg)减少可能会抑制供体NK细胞的增殖,也抑制可以应用的NK细胞治疗方案。最近的一项临床试验表明,用IL-2联合白喉毒素融合蛋白抑制宿主调节性T细胞可增加NK细胞的增殖并用来治疗成人复发性AML。
四、T细胞治疗进展
髓系细胞在免疫系统中的角色之一是其可能限制免疫系统识别白血病细胞。然而,机体并不存在完成的抗AML系统,特异性T细胞无法检测抗蛋白酶3、白细胞特异抗原(WT1)等。此外,一些数据表明,T细胞应答的程度与疗效呈正相关。这样的研究结果的解读需谨慎,该结果可能仅反映了肿瘤的免疫原性的差异与不同的生物或其他混杂因素的影响,而不能反应特异性T细胞反应在AML的进展。在造血干细胞移植后,异基因淋巴细胞大量扩增,从而增加了T细胞的免疫源性,以此有效治疗白血病并防治复发。但目前仍不清楚AML是如何在免疫系统的重塑下发生的,其机制仍需要进一步研究。
通过体外将白血病相关抗原转移至白血病特异型T细胞内可有效提高T细胞的肿瘤杀伤作用。T细胞免疫治疗的另一种方法是体外扩增肿瘤特异性T细胞,并转移到患者体内。激活抗原特异性T细胞输注不需要原位免疫刺激。为确保大量所需的特异性T细胞,可以通过修改这类细胞的基因以此促进TCR的增殖。扩增肿瘤特异性T细胞的研究已经在黑色素瘤和其他恶性肿瘤中得到证据。但与AML有关的研究数据还不完善。研究的前景依然具有吸引力,特别是考虑到存在白血病细胞的骨髓和其他造血器官在TCR增殖时可以带来的临床获益。
由于胸腺发育的限制,自体AML特异性TCR可能无法精准的杀伤白血病细胞。然而,TCR可以通过修改及重塑增强肿瘤免疫应答。免疫敏感性低的异种异体移植TCR可通过HLA转基因小鼠或其他品种的小鼠进行免疫处理从而得到亲和力更高的TCR的异种抗原免疫或其他物种形成可能允许高亲和力的TCR的生产。另外,研究人员采用结构分析和分子动力学鉴定氨基酸热点的存在,发现突变明显且稳定性高的TCRCDR3环可增加TCR结合自由能和亲和力。也有研究者通过体外进化技术产生高亲和力的TCR,重塑TCR的过程也必须谨慎,因为TCR基因突变也会产生新的性质,某种程度上会增加不良反应的发生率。事实上,TCR-MHC复合物多数是针对MHC而非其特异性抗原,一旦此类复合物表达增加可能会改变TCR识别能力,限制其与配体的结合。因此,在临床治疗前应彻底分析进行基因修饰后的受体的安全性。
TCR通常依赖CD4或CD8共受体识别抗原-MHC复合物。当亲和力增加,TCR可能将独立与共受体系统。增强TCR亲和力的治疗方案可以使CD4和CD8T细胞的识别功能增强。虽然对T细胞免疫治疗的主要执行者是CD8效应细胞,但近年来研究发现CD4T细胞也对某些肿瘤细胞具有杀伤作用,且对于CD8细胞的增殖有积极的意义。因此这2种类型的细胞共同移植对于AML的治疗是有利的。
1. T细胞免疫应答的限制
肿瘤细胞通过下调MHC分子表达以及降低抗原递呈进而发生免疫逃逸是T细胞治疗需要克服的难题。多数AML为程序性死亡受体(PD-L1)阳性,肿瘤细胞表达PD-L1和PD-2,与T细胞和NK细胞表达的PD-1结合后,对T细胞活化产生抑制性信号,下调SHP-2磷酸酶信号发生免疫逃逸。AML可以表达IDO,另一γ干扰素诱导基因,通过耗竭色氨酸降解副产物生成,抑制细胞免疫和促进调节性T细胞(Treg)的形成。大量的调节性T细胞可能在骨髓微环境中聚集,这些可以使AML细胞抑制CTLA-4的表达增加,增加腺苷产生及其他机制。考虑到多个抑制性信号抑制T细胞过继转移,联合免疫治疗将可能是未来发展的一个趋势。PD-1阻滞剂nivolumumab治疗AML的研究也在进行。类似于靶向PD-1的抗体,负性T细胞调节因子CTLA-4的抗体可用于治疗AML。CTLA-4通过2种机制抑制T细胞活化,一是T细胞活化时CTLA-4表达增加,与其受体CD80和CD86相互作用可抑制T细胞活化。二是CTLA-4构成性表达于调节性T细胞(Tregs),在免疫抑制中发挥关键性作用。
Tregs以CTLA-4依赖方式下调DSs中CD80和CD86,使得DCs不能启动免疫反应。CTLA-4抗体ipilimumab被批准用于转移性恶性黑色素瘤,一些临床试验显示能改善患者总生存。有报道显示Tregs数量增多与AML不良结局具有相关性。靶向CTLA-4治疗AML的早期试验正在进行。
成功的细胞疗法可使移植的T细胞具有更长的作用效果。治疗性T细胞的增殖动力、肿瘤细胞消亡及临床疗效之间的联系,可能与传统的依靠药代动力学与药效学定义的生物制剂有很大的不同。目前研究发现AML患者体内的T细胞抗原决定簇不是肿瘤特异性,任何成功的细胞免疫治疗都可能增加延长骨髓抑制的风险。研究证实细胞毒治疗可以消除相关风险,并可以在造血干细胞移植前将“自杀基因”dimerizableHSV-TK和caspase9植入细胞内。
2. 嵌合抗原T细胞
嵌合抗原受体T细胞(CAR-T)是将能识别某种肿瘤抗原的抗体的抗原结合部与CD3-ζ链或FcεRIγ的胞内部分在体外偶联为一个嵌合蛋白,通过基因转导的方法转染患者的T细胞,使其表达CAR。
当患者自身T细胞被重新修饰后则产生大量肿瘤特异性CAR-T。CAR包含有细胞外抗原结合域、跨膜域、信号细胞内结构域。胞外结构域是典型的单链可变片段(scFv)源于肿瘤特异性单克隆抗体。应用抗体衍生的结构域识别抗原有3个优点:
①抗体不依赖MHC递呈,即CARs为非HLA限制性,不承担与内源性TCR链错配的任何风险;
②抗体结合抗原比TCARs有更高的亲和力,形成更稳定的免疫突触;
③治疗更精准,由于CAR-T细胞是应用基因修饰患者自体的T细胞,利用抗原抗体结合的机制,能克服肿瘤细胞通过下调MHC分子表达以及降低抗原递呈等免疫逃逸,让肿瘤细胞无所逃遁。
CAR-T细胞的临床疗效首先在B细胞恶性肿瘤中得到证实。CD19-41bb-ζ CAR-T,是最开始进行临床应用的,随后CD19-CD28-ζ CAR由Brentjens和Sadelain用于治疗难治性急性淋巴细胞白血病和更成熟的B细胞白血病/淋巴瘤。上述发现使得CAR-T治疗髓细胞白血病成为一种可能。除了CD19-CAR的初步成功,其他CAR-T也被临床研究证实有效。目前对于CAR治疗的不良反应报道主要为体内可能会产生抗CAR抗体、细胞因子释放综合征等,如果处理不当会严重威胁患者的生命。设计CAR识别区域是CAR治疗前的重要先决因素。目前研究人员将重点放在用CD33-CAR治疗AML。在体外和临床前实验中证实CD33-CAR-T细胞具有较好的疗效。CD33在绝大多数的白血病细胞中均有表达,且在造血干细胞中无表达。初步研究中发现1例患者可被CD33-CAR治愈。此外CD44v6、CD123等AML干细胞抗原也被发现可用于替代CD33。
有研究测试了二代CD123 CAR-T细胞,它是由1个CD123 CAR和CD28共刺激分子组成。这种CAR-T细胞在异基因小鼠体内表现出了有效的抗白血病效应,而且在体外实验中发现,利用AML患者T细胞制作成的CD123 CAR-T细胞能够重新杀伤患者自身的白血病细胞。他们还将CD123CAR-T细胞与脐血中的CD34+细胞共培养,仍然能培养出正常的细胞集落,提示CD123 CAR-T细胞对脐血中CD34+细胞并没有杀伤作用。Tettamantis等也在细胞因子诱导的杀伤(CIK)细胞上加上了一代CD123 CAR,即一代CD123 CAR CIK细胞,证实了CD123 CAR-T的抗白血病效应及靶向性。然而,目前尚无CD123 CAR-T成功治疗AML患者的报道,究其原因可能如下:
①最佳的CAR设计尚不清楚。例如如何选择共刺激分子及其数量、细胞膜外连接片段的长度等。
②CAR-T细胞的制备技术尚不成熟。
③CAR-T细胞在体内的存在时间尚无法合理控制。
④不良反应。目前临床上报道的不良反应主要有B淋巴细胞“再障”、细胞因子释放综合征及神经系统毒性。
⑤无法有效克服肿瘤微环境的抑制作用。因此,治疗过程需在有丰富免疫治疗经验的医生指导下进行,以降低治疗风险。
目前研究也在更积极的开拓可与CAR联合的抗原,包括PD-L1、IDO及一些抑制因子等。AML是一种多样化的髓样癌,因此无法通过单一靶点治疗所有的临床亚型。有效的治疗应可以清除发生转化的肿瘤干细胞,同时清除由此干细胞分化而成的下一代细胞,因此所需设计的区域则更为复杂多变。
五、结论
在过去的几十年,AML的基础治疗方案未发生重要的突破。虽然个体化治疗、替代治疗等方式取得了一定的进步,但仍不足以满足AML的治疗需要。免疫治疗,通过攻击肿瘤的抗原结构,未来可能作为现有治疗方案的补充方案。目前的研究也证实免疫治疗的疗效取得了突破性的进展,今后应在发挥自身优势的情况下,最大限度地减少治疗的毒副作用,与常规治疗有效结合更好的治疗AML并预防复发。
来源:中华全科医学.2017.15(10):1763-1767
原标题《急性髓系白血病免疫治疗方式及研究进展》
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#髓系白血病#
31
内容丰富.值得学习
60
谢谢分享.学习了
67
学习了分享了
70
学习了新知识
59
好好好好好好好好
66
谢谢分享.阅读
28
谢谢了.学习
21