Neurocrit Care:神经源性应激性心肌病1例
2018-06-02 杨中华 脑血管病及重症文献导读
76岁,女性。因为突发剧烈头痛收住NCU治疗。 CT显示弥漫性蛛网膜下腔出血(SAH),伴脑室积血和脑积水。Hunt-Hess评分2分,mFisher评分3分。CTA显示右侧脉络膜前动脉动脉瘤。入院时神经系统查体完成正常,但是入院后很快出现昏睡。随后放置脑室外引流(EVD),测压力为22 cmH2O。患者逐渐清醒,并进行了动脉瘤弹簧圈栓塞术。脑室外引流的引流高度保持在15 cmH2O,并且每
76岁,女性。因为突发剧烈头痛收住NCU治疗。
CT显示弥漫性蛛网膜下腔出血(SAH),伴脑室积血和脑积水。Hunt-Hess评分2分,mFisher评分3分。CTA显示右侧脉络膜前动脉动脉瘤。入院时神经系统查体完成正常,但是入院后很快出现昏睡。随后放置脑室外引流(EVD),测压力为22 cmH2O。患者逐渐清醒,并进行了动脉瘤弹簧圈栓塞术。脑室外引流的引流高度保持在15 cmH2O,并且每天在物理治疗师的指导下在走廊走动。经胸超声提示射血分数65%,无其他异常。
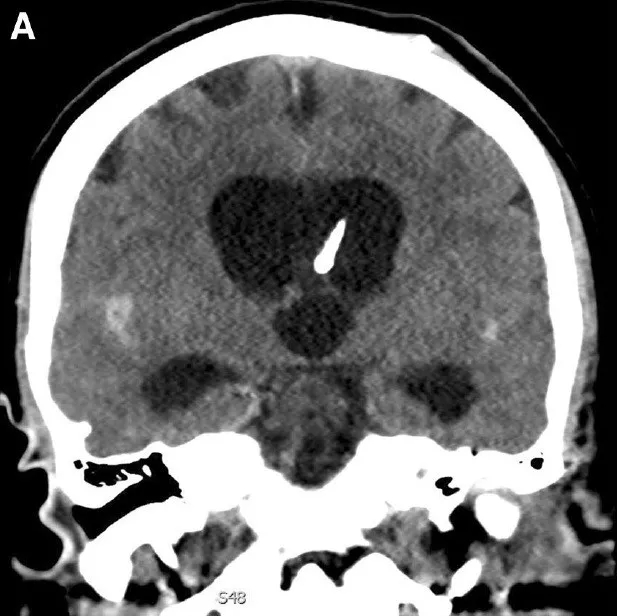
EVD高度维持在15 cmH2O,脑脊液引流量从最初的186 ml/24 逐渐减少到夹闭前69 ml/24h。夹闭前,颅内压为0-10 mmHg,平均6 mmHg。出血后第6天早上夹闭EVD。晚上,患者头痛加重,睡眠增多,定向力障碍。CT显示脑室扩大(下图),此时颅内压为2-20 mmHg,平均7.8 mmHg。颅内压波形提示顺应性不良,P2波高于P1波。再次打开EVD,压力引流高度控制在15 cmH2O。夜间,患者的精神状态持续恶化。CTA和灌注影像未发现血管痉挛或灌注下降。第7天早上,患者深度昏睡状态(deeply stuporous),向下凝视,并进行气管插管。复查CT显示脑积水加重。EVD引流高度设置为0 cmH2O。
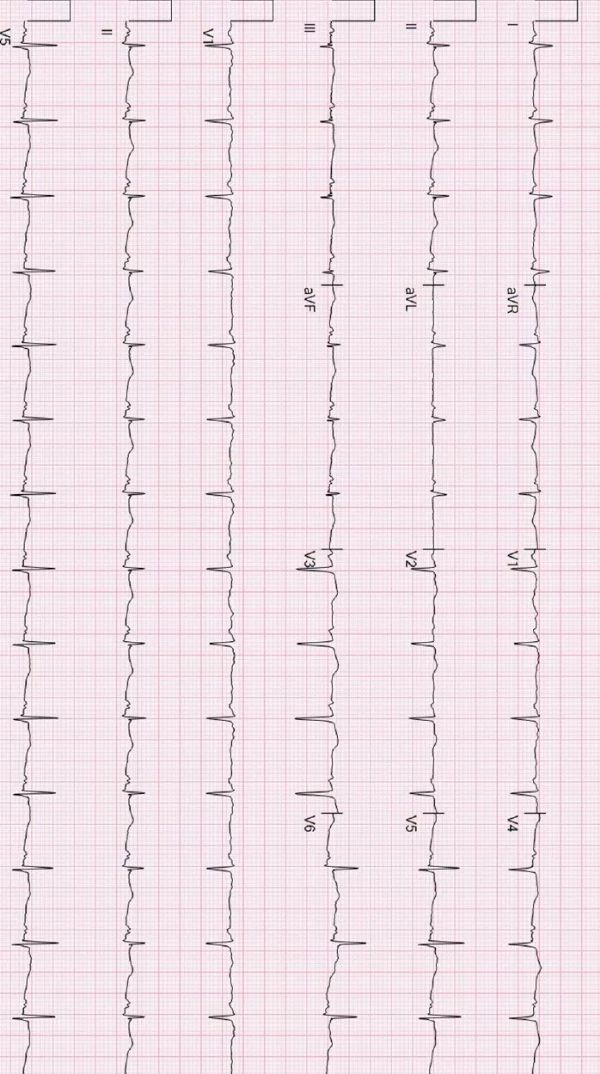
患者开始出现低血压。心电图显示急性冠脉综合征,下侧壁ST抬高1mm(下图),提示可能为心肌梗死。肌钙蛋白5.97,CK-MB 21.4。血压越来越低,静脉输液无效,需要升压药物维持血压。复查经胸超声心动图显示射血分数为35%,前间隔远侧、前壁远侧、下壁远侧和心尖运动不良(下图)。急诊心脏导管仅见轻度轻度冠脉病,未见血管闭塞,符合应急性心肌病的表现。
第8天神经系统查体恢复到基线状态,复查CT显示脑积水改善(下图)。第9天拔除气管插管,脑室腹膜分流术,拔除EVD。21天复查超声心动图显示射血分数为65%,没有其他异常。
讨论:
报道显示,28%动脉瘤蛛网膜下腔出血会伴发神经源性应激性心肌病(Neurogenic stress cardiomyopathy,NSC),通常发生在出血第二天。高Hunt-Hess分级是NSC的强预测因子。治疗性高血压预防迟发性脑缺血的患者也会发生NSC,是一种迟发性NSC,升压药物的剂量时神经源性心脏损伤的独立预测因子。本例患者在第7天发生NSC,当时未使用升压药物,作者认为当时的进展性脑积水是NSC的诱发因素。
急性脑积水相关NSC报道很少,其中两个病例报道为三脑室囊肿。这三例报道的机制可能为高颅内压引起交感肾上腺功能活动过度,导致儿茶酚胺过度分泌。本例报道的独特之处为NSC前和NSC过程中一直进行了颅内压监测,脑积水后,颅内压未升高。因此颅内压升高可以引起NSC,但是颅内压升高并不是必须的。即使引流期间平均颅内压正常的情况下,顺应性降低也会引起症状性脑积水,增加NSC的风险。
位于下丘脑的控制交感神经重要结构毗邻三脑室。下丘脑室旁核和背内侧核与儿茶酚胺-诱导心肌坏死有关。作者认为,脑积水会破坏神经心脏调节中枢,与颅内压无关。
该病例的两个亮点为:1.提醒临床医生脑积水可能是NSC的诱发因素;2.颅内高压并不是NSC的必须条件,特别是合并脑积水时。
原始出处:
Kamel Gharaibeh, et al.Neurogenic Stress Cardiomyopathy Precipitated by Acute Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage.Neurocrit Care. 2018 Apr;28(2):239-242. doi: 10.1007/s12028-017-0437-0.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ROC#
33
#神经源性#
41
#神经源#
37
#应激性心肌病#
37
#应激#
21
#肌病#
27
认真学习.不断进步.把经验分享给同好.点赞了!
55