盘点:卵巢癌2016年重要研究进展
2016-08-15 MedSci MedSci原创
众所周知,卵巢恶性肿瘤是女性生殖器官常见的恶性肿瘤之一,发病率仅次于子宫颈癌和子宫体癌而列居第三位。但卵巢上皮癌死亡率却占各类妇科肿瘤的首位,对妇女生命造成严重威胁。这里小M盘点了今年以来卵巢癌方面的重要研究进展与大家分享。 【1】 Cell子刊发表两项卵巢癌研究进展 最近来自英国牛津大学的一支研究团队在EBioMedicine和Cancer Cell两个国际学术期刊上发表了两项卵
众所周知,卵巢恶性肿瘤是女性生殖器官常见的恶性肿瘤之一,发病率仅次于子宫颈癌和子宫体癌而列居第三位。但卵巢上皮癌死亡率却占各类妇科肿瘤的首位,对妇女生命造成严重威胁。这里小M盘点了今年以来卵巢癌方面的重要研究进展与大家分享。
【1】 Cell子刊发表两项卵巢癌研究进展
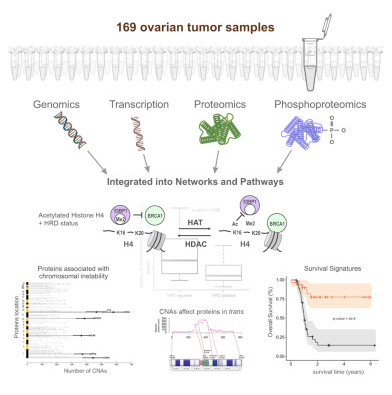
最近来自英国牛津大学的一支研究团队在EBioMedicine和Cancer Cell两个国际学术期刊上发表了两项卵巢癌研究进展,他们在第一项研究中发现了一个帮助早期检测卵巢癌的标志物分子,并在第二项研究中发现一种使卵巢癌变得更加致命的关键酶。
在第一项研究中研究人员发现SOX2的蛋白表达水平在卵巢癌患者输卵管中的水平更高,并且在一些卵巢癌高危人群(如BRCA1和BRCA2基因突变携带者)中SOX2的表达水平也会更高。
在第二项研究中,该研究团队发现了一种促进卵巢癌细胞扩散的关键酶。当卵巢癌发生扩散,通常会扩散到网膜——覆盖小肠的脂肪组织。卵巢癌患者最常见的死因就是肿瘤生长阻塞肠道导致的营养不良。
研究表明SIK2不仅在卵巢肿瘤的生长过程中发挥关键作用,还在卵巢肿瘤向网膜的扩散过程中发挥重要作用,这会使卵巢癌变得更加致命。
研究人员表示,SIK2不仅能够为癌细胞提供能量,还会进一步增加癌细胞的数目,因此是未来卵巢癌治疗的一个重要靶点,破坏这种关键酶能够降低癌细胞扩散和癌症复发的可能。(文章详见——牛津大学科学家Cell子刊发表两项卵巢癌研究进展)
【2】 缺乏锻炼与卵巢癌的发病风险增加有关
两项新研究提示着缺乏锻炼与患上卵巢癌风险和死于卵巢癌的风险增加相关联。这两项研究分别发表在Cancer Epidemiology, Biomarkers & Prevention期刊和British Journal of Cancer期刊上。
在第一项研究中,研究人员分析了8300多名卵巢癌患者和12600多名未患上卵巢癌的女性。研究人员发现,相比于那些开展规律性锻炼的女性而言,那些说她们在她们的生命当中未开展娱乐性体力活动的女性患上卵巢癌的风险增加了34%。
根据这项研究,缺乏锻炼与更高的卵巢癌风险之间的关联性是在正常体重的女性和超重或肥胖的那些女性中观察到的。
第二项针对6800多名卵巢癌患者的研究发现在确诊卵巢癌多年前缺乏锻炼的女性要比那些开展至少一些每周规律性锻炼的女性死于卵巢癌的风险增加了22%~34%。
研究人员表示,不到45%的卵巢癌患者能够存活5年。尽管这两项研究并不能够证实锻炼能够阻止这些癌症死亡病例,但是它们提示着规律性锻炼可能是有益处的。(文章详见——两项新研究揭示锻炼可能有助阻止卵巢癌)

【3】 铂敏感复发的卵巢癌接受Olaparib维持治疗可以获得长期生存获益
Study19研究的进一步随访数据显示,铂敏感复发的卵巢癌接受Olaparib维持治疗可以获得生存获益,Olaparib耐受性可,可用于长期维持。
患者1:1随机接受Olaparib(400 mg bid, 胶囊)或安慰剂治疗,其中,96%(254/265)的入组患者BRCA突变状态明确。结果,无论是FAS还是BRCAm亚组,接受Olaparib相比于安慰剂组,均显示出了OS优势;FAS集患者的生存获益可能主要由于BRCAm患者的OS获益所致。
在FAS人群,Olaparib和安慰剂组5年的生存率分别为29.2%和20.4%;BRCAm亚组,5年的生存率分别为36.9%和24.3%. 截至2015年9月30日,Olaparib组15例(BRCAm 8例)和安慰剂组1例(BRCAm 1例)仍在接受治疗。Olaparib组中,13.2%(18/136)的患者接受了5年以上的Olaparib治疗(其中,BRCAm患者11例;non-BRCA突变患者7例)。(文章详见——ASCO 2016:奥拉帕利(Olaparib)全面开战:卵巢癌、乳腺癌、胃癌)
【4】每周一次 vs 每3周一次紫杉醇治疗卵巢癌无显著效果差异
据发表于NEJM的一项研究表明,每周接受一次紫杉醇的卵巢癌患者与每3周接受一次紫杉醇治疗的患者相比,并没有延长无进展生存期。
每周密集剂量服用紫杉醇(服用药物的频率更大)加上每3周服用一次卡铂,或者在紫杉醇中加入贝伐单抗和每3周服用卡铂治疗卵巢癌已显示出功效。研究人员旨在确定在那些接受和没有接受贝伐单抗的患者中,每周服用密集剂量紫杉醇和卡铂的患者与每3周服用一次紫杉醇和卡铂的患者相比,是否会延长无进展生存期。
共有692例患者参与研究,84%的患者选择接受贝伐单抗。在意向治疗分析中,每周接受紫杉醇治疗与每三周接受紫杉醇治疗的患者相比,每周服用紫杉醇并没有延长无进展生存期。在没有接受贝伐单抗的患者中,每周接受紫杉醇与每3周接受紫杉醇治疗的患者相比,无进展生存期延长了3.9个月。然而,在接受贝伐单抗的患者中,与每3周服用一次紫杉醇相比,每周接受紫杉醇的患者没有显著延长无进展生存期。一个互动评估的治疗效果同质化测试显示出接受贝伐单抗治疗和没有接受贝伐单抗治疗的患者之间有显著的差异。每周接受一次紫杉醇的患者比那些每三周接受一次紫杉醇的患者有较高的3或4级贫血事件发生率,以及更高2〜4级感觉神经病变发生率;然而,他们有较少的3或4级中性粒细胞减少事件发生。(文章详见——
NEJM:服用紫杉醇的频率(每周一次 vs 每3周一次)对于治疗卵巢癌无显著效果差异)

【5】卵巢癌新药Farletuzumab三期临床试验结果失败
Farletuzumab是一种人源化的单克隆抗体,其靶点为叶酸受体α。叶酸受体α在卵巢癌中高度表达而在大部分正常组织中并不存在。Farletuzumab目前处于双盲、随机的三期临床试验中,用于治疗对铂敏感性卵巢癌。
符合试验条件的患者是在经过铂-紫杉烷化疗完成后出现首次复发6-24个月。所以的患者均接受卡铂加紫杉醇或者多系紫杉醇(六个循环结合随机分配的测试药物,比例为1:1:1,Farletuzumab 1.25mg/kg,2.5mg/kg或者的安慰剂)。单药物测试每周都进行直到疾病进展。主要的结束终点是根据实体瘤反应评价条件确定的无进展生存时间(PFS)。
共有1100名女性参与此次研究。随机分组,接受治疗剂量或者安慰剂给药治疗。对于上述给药方案,从最初分析得到的PFS分别为9.5、9.7和9.0个月。单抗组无论是哪一种剂量都和安慰剂对照组没有显著性差异。在预先设定的亚组中,基线CA-125水平不高于正常的上限的三倍。Farletuzumab暴露的亚组分析表明相对于安慰剂,这种单抗有着更好的PFS。试验中最常见的不良事件都是和化疗相关的。这些研究表明,单抗的两种剂量都可以没有达到主要PFS终点的要求。(文章详见——JCO:卵巢癌新药Farletuzumab三期临床试验结果发表,3年前已完成试验,结果阴性)
【6】重视卵巢癌的筛查以降低死亡率
伦敦大学学院研究的卵巢癌筛查试验新结果表明,筛查基于每年的血液测试可以帮助减少疾病造成的20%左右的死亡率。
超过200000名年龄在50到74岁之间,没有卵巢癌家族遗传史的绝经后妇女参与了这一研究。他们被随机分配到三组:多通道筛选或阴道超声波,直到2011年12月前她们都要接受每年一次的检查,对照组不进行检查。直到2014年12月研究结束前诊断出1282名妇女中的649人死于这种疾病。
早期的结果表明, 每10000名女性参加筛查计划,包括在7至11年间的年度血液测试中大约有15人可以预防因卵巢癌而死亡。(文章详见——The Lancet:卵巢癌筛查可救命)
【7】60岁以上的卵巢癌的BRCA+患者预防性切除乳房或并不会获益
来自杜克大学医学中心产科学及妇科肿瘤学住院医师Charlotte R. Gamble和同事对BRCA+的卵巢癌患者进行了一项研究,发现60岁前诊断为卵巢癌的BRCA+患者,进行预防性乳房切除术可延长生存,每年的费用也在可接受范围,但是对于60岁以上的高危卵巢癌患者,无论是医学还是经济上,进行乳房切除均不划算,延长的生存时间很短很有限,但是付出的金钱却很多。
研究数据显示,对40岁确诊为卵巢癌的BRCA1+患者,预防性乳房切除可延长8个月的生存(相比乳腺筛查),多出来的生存时间里,成本有效性比率(ICER)增加$12,298/年;对于50岁确诊为卵巢癌的BRCA1+患者,预防性乳房切除可延长6个月的生存,ICER增加$24,255/年;对于60岁确诊为卵巢癌的BRCA1+患者,预防性乳房切除可延长3个月的生存,ICER增加$56,881/年;对于70岁确诊为卵巢癌的BRCA1+患者,预防性乳房切除可延长1.5个月的生存,ICER增加$143,207/年。
分别在40岁、50岁、60岁和70岁诊断为卵巢癌的BRCA2+患者,进行预防性乳房切除分别可延长7个月、5个月、3个月和2个月的生存。这类患者中,≤60岁的患者进行乳房切除具有成本有效性,但是对于70岁的患者,则不具有,其ICER增加$119,557/年。
此外,研究者发现,对40岁诊断为卵巢癌的患者进行乳房切除,多存活的日子里每年花费少于$100,000的可能性为99%。到70岁,BRCA1+患者的花费可降低24%,BRCA2+患者的花费可降低36%。(文章详见——卵巢癌患者该不该预防性切除乳房?年龄也是一个坎)

【8】2016 NCCN临床实践指南:遗传/家族高风险评估-乳腺癌和卵巢癌(2016.V2)
2016年3月美国国家综合癌症网络(NCCN)发布了遗传/家族高风险评估-乳腺癌和卵巢癌指南2016年第2版。指南更新摘要为:
乳腺癌和/或宫颈癌的遗传学评估
BRCA相关性乳腺癌和/宫颈癌综合征
BRCA突变阳性的管理
李法美尼症候群的管理
Cowden综合征/错构瘤肿瘤综合症的管理
多基因检测
乳腺癌/宫颈癌相关额外基因突变的例子

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
48
#研究进展#
26
继续学习
47
继续关注
49
学习学习!
59
学习起来
47
继续关注
28
继续学习
30