凶险性前置胎盘围手术期的处理
2020-07-06 邓友明 张娟 张维峰 临床麻醉学杂志
随着二孩政策的放开,二胎产妇在各地都有较快的增长,这也导致疤痕子宫需要剖宫产的产妇不断增加,疤痕子宫合并完全性前置胎盘并植入的产妇势必增加。前置胎盘合并植入是产妇围生期大出血的高危因素,以往报导多以切
随着二孩政策的放开,二胎产妇在各地都有较快的增长,这也导致疤痕子宫需要剖宫产的产妇不断增加,疤痕子宫合并完全性前置胎盘并植入的产妇势必增加。前置胎盘合并植入是产妇围生期大出血的高危因素,以往报导多以切除子宫来保住产妇生命。目前,随着对这类产妇病理生理改变认识的提高,以及麻醉技术、手术技术和介入技术的水平提高,这类产妇围生期死亡率、子宫切除率大大降低。现将2017年处理的8例产妇经验体会叙述如下。
1.资料与方法
一般资料:本院诊断为凶险性前置胎盘的产妇8例,年龄28~40岁,体重65~85kg,BMI25~31kg/m2,ASAⅡ或Ⅲ级。所有产妇均为剖宫产后妊娠,时间间隔2~10年,均为单胎妊娠。
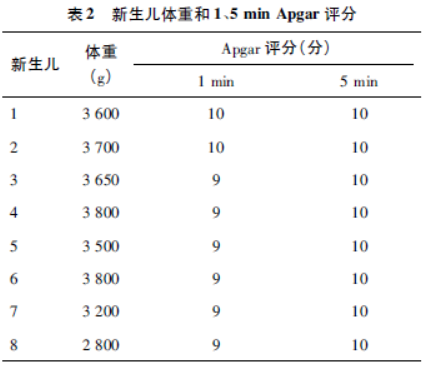
方法:住院产妇择期剖宫产前先在介入科放置主动脉球囊阻断器,后立即入手术室准备剖宫产。急诊出血入院直接入手术室,在手术室放置主动脉阻断器。产妇入室后,监测BP、ECG、SpO2,有创动脉穿刺测压、深静脉置管,建立18号外周静脉通路,术前备红细胞3U、血浆600ml、冷沉淀10U,白蛋白100ml,凝血酶原复合物等凝血物质,8例产妇均先予腰硬联合椎管内麻醉,重比重0.5%布比卡因2ml蛛网膜下腔给药,平面控制在T6以下,硬膜外置管必要时给予2%利多卡因,7例在腰硬联合麻醉下完成手术,1例取出胎儿后因出血多加用气管插管全身麻醉,术中根据出血情况补充红细胞和凝血物质。6例取出胎儿后立即使用了主动脉阻断器,2例术中没有使用阻断器,没有子宫动脉结扎,术后出血也不多。8例均行子宫绑扎,6例行子宫动脉结扎术,4例产妇在术中行子宫动脉栓塞术;2例术后行子宫动脉栓塞术,1例切除子宫。术毕1例产妇入ICU,余7例送回病房。观察指标:记录产妇麻醉方式,出血量,子宫处理情况,是否使用阻断器,术中输血情况,术后是否入ICU。记录新生儿体重和1、5minApgar评分。
2.结果
8例产妇中因孕期出血有3例于33周入院保胎治疗至36周择期剖宫产,4例提前1周入院保胎治疗。所有产妇入室情况均较平稳。麻醉方法,术中出血量,子宫结局、阻断器使用情况和入ICU情况见表1。7例产妇术后血流动力学平稳后送回病房,术中出血1000ml以上的产妇中有3例均输入红细胞3U和血浆400ml,另有1例出血8000ml以上的产妇在取出胎儿后开始输红细胞12U、血浆2000ml、冷沉淀10U、血小板1个治疗量、凝血酶原复合物2U,该产妇切除子宫,术后送入ICU,第2天生命体征平稳送回普通病房。8例产妇均康复出院。8例新生儿情况均较好,体重均大于2500g,1、5minApgar评分均在9分以上(表2)。

3.讨论
凶险性前置胎盘是指胎盘附着于前次剖宫产子宫切口瘢痕处,伴或不伴有胎盘粘连、胎盘植入。有报道前次剖宫产发生胎盘植入率高达30%~50%,病死率10%。凶险性前置胎盘尤其合并胎盘植入者出血汹涌,止血困难。
研究表明,剖宫产次数与前置胎盘发生率相关性很大,1次剖宫产再次妊娠发生前置胎盘的概率是无剖宫产史再次妊娠的5.3倍,其发生胎盘植入的概率则是无剖宫产史的35倍。其发生机制可能主要是与子宫瘢痕处子宫内膜受损,切口瘢痕行成有关。不可预知、不可控制的产时、产后出血是凶险性前置胎盘对于孕产妇最主要的威胁。因此对此类产妇的围产期管理显得尤为重要,手术管理的原则:
(1)尽量不做急诊剖宫产、尽量清除胎盘组织、术前做好防止出血的准备、备好血源。对凶险性前置胎盘孕妇,会根据其是否有产前出血情况而决定住院孕周,终止妊娠时间一般选择在36周左右以利于胎儿肺发育成熟。术前准备包括介入科置入主动脉球囊阻断器预防胎盘取出时的出血,而麻醉科做好大出血的准备,包括血液制品,输液通路,气道快速建立方案,麻醉科医师人员配备。
(2)术中产科医师可以在进入腹腔后根据子宫表面情况初步预估手术的难易程度,确定是否在取出胎儿后立即行主动脉阻断以预防出血。盆腔粘连严重、子宫下段菲薄、局部见怒张血管或肌层组织薄弱、隐约可见胎盘组织向宫壁凸起时,切开子宫时需尤为慎重,把备好的血源拿到手术室后方可切开子宫,术中要充分剥离胎盘组织,缝合子宫预防性行子宫绑扎,主动脉阻断器的使用可以为凶险性前置胎盘剥离和子宫缝合时期减少出血,而子宫动脉栓塞有效的阻止了大多凶险性前置胎盘的出血,而保全子宫不被切除。
术中麻醉管理的重点是对大出血的处理,术前凝血物质的准备是必备的,麻醉方式,术前做全麻准备是应对不可控出血时必须的,维持术中血流动力学的稳定,维护大出血产妇的凝血功能可以减少出血,输血科的积极配合也很重要;术中麻醉管理、阻断器的使用、子宫动脉结扎、子宫动脉栓塞联合使用可以减少出血,可降低子宫切除率。综上所述,凶险性前置胎盘围手术期的处理,剖宫术前放置阻断器、术中血流动力学的稳定、术中凝血功能的维护、术中子宫动脉的结扎、子宫动脉的栓塞可减少出血,降低子宫切除率。麻醉的选择,手术场地的选择,射线的防护,阻断器的使用、肝素化,术中血液制品输入的时机以及血气监测和出凝血功能监测与治疗等有待进一步的改善。
原始出处:
邓友明,张娟,张维峰,仲艳玲,白淑芬,戴峰.凶险性前置胎盘围手术期的处理[J].临床麻醉学杂志,2019(07):701-702.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了
36
#手术期#
34
#前置胎盘#
45
#胎盘#
41
学习了
82