低龄原发腮腺多形性腺瘤1例
2018-12-28 胡琛 张磊涛 罗醒红 分子影像学杂志
患儿,男性,14岁,主因左侧耳垂下肿物3年余入院。患者于3年前无明显诱因发现左侧耳垂下出现一肿物,约“蚕豆”大小,无痛,未予重视,未予治疗。后发现该肿物渐进性增大至“荔枝”大小。今为进一步治疗来我院门诊就诊,双侧涎腺B超结果示:(1)左侧腮腺混合性回声团伴多发钙化,建议进一步检查;(2)右侧颈部Ⅱ区见异常淋巴结;(3)右侧腮腺及双侧颌下腺未见明显异常;(4)左侧颈部淋巴未见明显异常淋巴结回声。门诊
多形性腺瘤又称良性混合瘤,是最常见的唾液腺肿瘤,可发生于各唾液腺体,最常见于腮腺。腮腺多形性腺瘤属于临床常见良性肿瘤,好发于中老年患者,罕见低龄患者。本文通过报道1例低龄原发腮腺多形性腺瘤的诊疗经过,并结合本院2005~2017年就诊的低龄原发腮腺多形性腺瘤资料及文献复习,讨论该疾病的临床特征、术式选择及与年龄的关系。
1.病例资料
患儿,男性,14岁,主因左侧耳垂下肿物3年余入院。患者于3年前无明显诱因发现左侧耳垂下出现一肿物,约“蚕豆”大小,无痛,未予重视,未予治疗。后发现该肿物渐进性增大至“荔枝”大小。今为进一步治疗来我院门诊就诊,双侧涎腺B超结果示:(1)左侧腮腺混合性回声团伴多发钙化,建议进一步检查;(2)右侧颈部Ⅱ区见异常淋巴结;(3)右侧腮腺及双侧颌下腺未见明显异常;(4)左侧颈部淋巴未见明显异常淋巴结回声。门诊以“左侧腮腺良性肿物”收入院。自发病以来,患儿精神状态良好,食欲食量正常,睡眠情况良好,体质量无明显变化,大小便正常。
专科检查:患者无明显面神经麻痹症状,左侧腮腺后下极可扪及一肿物,大小约3 cm×3 cm×4 cm,表面皮肤颜色及皮温正常,质地偏硬,活动度一般,边界清晰,与周围皮肤无黏连,未扪及波动感及搏动感。双侧颞下颌关节无弹响,无压痛,开口度及开口型基本正常。颏下、双侧下颌下及颈部未扪及明显肿大淋巴结。
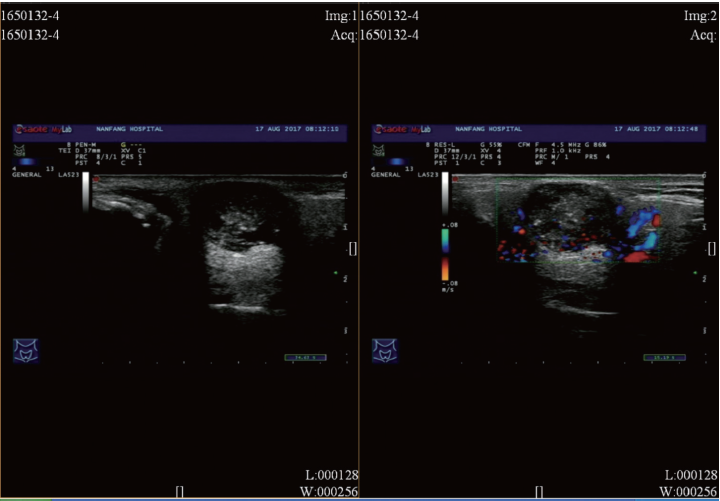
口内检查:口腔卫生情况可,口内黏膜未见明显异常。双侧腮腺导管口无红肿,挤压腮腺可见清亮液体流出,舌质软,活动度正常,伸舌居中无偏斜。辅助检查:2017年8月17日我院双侧涎腺及颈部B超结果示(图1):(1)左侧腮腺混合性回声团伴多发钙化,建议进一步检查;(2)右侧颈部Ⅱ区见异常淋巴结;(3)右侧腮腺及双侧颌下腺未见明显异常;(4)左侧颈部淋巴未见明显异常淋巴结回声。
图1 术前B超结果
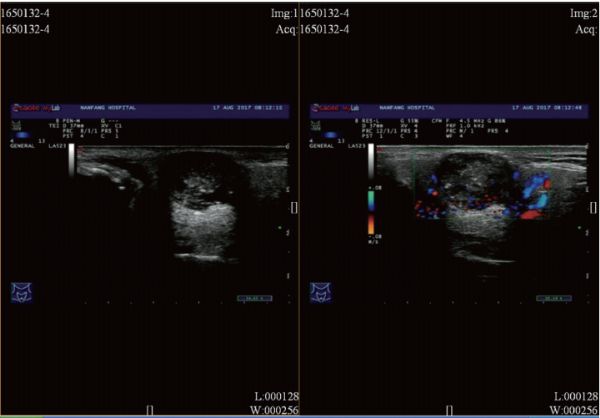
2018年8月22日我院双侧涎腺CT结果示(图2):左侧腮腺占位,考虑腮腺多形性腺瘤可能性大。初步诊断:左侧腮腺肿物(良性可能性大)。手术方案:左侧腮腺肿物切除术+面神经松解术。术中情况:(1)全麻显效后垫肩颈,头偏健侧,常规消毒铺巾;(2)于左侧耳垂后沿下颌骨下缘约2 cm,设计弧形切口,长约5 cm;(3)切开皮肤、皮下组织及部分颈阔肌,沿腮腺咬肌筋膜浅面向前翻开皮瓣,暴露肿物,见肿物呈白色,边界清晰,包膜完整,与面神经无黏连,保护好面神经下颌缘支,在肿物包膜外正常组织内将肿物完整切除;(4)切除肿物呈灰红色类圆形组织,大小约2.2 cm×1.8 cm×1.2 cm,切面灰白色,质地中等,边界清。送冰冻及常规病理,术中冰冻结果示:(左侧腮腺)多形性腺瘤;(5)术区置大清生物纸1张,并放置橡皮引流片,分层缝合颈阔肌、皮下组织及皮肤;(6)手术过程顺利,术中未损伤重要神经及血管,术中出血约10mL。
图2 术前CT结果
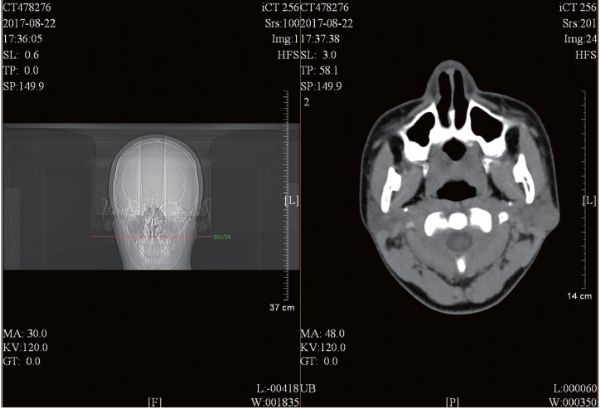
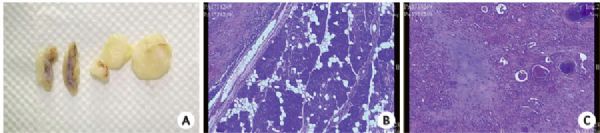
术后病理结果:术后常规病理结果(图3)示:(左侧腮腺)组织呈多结节状,其内可见瘤细胞排列呈片巢状或条索状结构,部分瘤组织向纤维包膜内生长;部分区域粘液变形,部分区域胶原化明显,并可见软骨样基质及钙化灶。(左侧腮腺)多形性腺瘤。最终诊断:左侧腮腺多形性腺瘤术后随访:术后1周复查,见左侧腮腺区无明显渗出红肿,术区可吸收缝线部分存,面部无面神经麻痹症状,颜面部无麻木不适。术后2周复查见:左侧腮腺区无明显渗出红肿,术区无缝线存,可见疤痕。
图3 肿瘤切片肉眼观(A)及显微镜下观(B、C)
2.讨论
2.1腮腺多形性腺瘤的年龄分布特点
多形性腺瘤好发年龄为30~60岁,女性患者多见,多形性腺瘤虽为良性肿瘤,但存在复发的可能,且具有癌变的潜在危险。其中,腮腺多形性腺瘤在各唾液腺中占比最高,也因此成为近年来的研究热点。但现有对于腮腺多形性腺瘤低龄患者的相关临床报道及研究较少,这也与其在临床较低的发病率有一定的关系。
腮腺多形性腺瘤的好发年龄为41~50岁的中年患者,极少发生于未成年低龄患者,唾液腺肿瘤在儿童中罕见,发病率与成人不同。本研究在收集南方医院2005~2017年间低龄患者资料时,也发现相似趋势。首先,低龄患者在临床较为罕见,在对南方医院13年来收治腮腺多形性腺瘤患者的数据进行统计时,发现仅有14例为未成年低龄患者(<18岁);其次,未成年患者人群中,0~6岁患儿占比最小(0%),6~12岁占比其次(14%),12~18岁占比最大(86%),即年龄越小,病例资料越罕见;第三,在这14例低龄腮腺多形性腺瘤人群中,男女比例为1:1,性别分布大致平衡。上述结论均提示:腮腺多形性腺瘤在低龄患者中可能存在与高龄患者不一样的临床分布特点。
2.2腮腺多形性腺瘤的复发性及其与年龄的关系
罹患原发性多形性腺瘤时患病年龄较小的患者群体,相比于成年患者,前者的复发率更高。其它相关研究也得出类似的结论:即原发性多形性腺瘤的低龄性是导致其复发率增大的危险因素之一。腮腺多形性腺瘤在低龄患者中存在与高龄患者不一样的临床特点。在临床应尤其重视对低龄原发多形性腺瘤的治疗,这对预防其复发有着重要的意义。对低龄患者腮腺肿瘤进行相关临床报道及研究很有必要。故针对低龄原发腮腺多形性腺瘤患者,选择适当的手术方式,从而有效降低其术后复发率,相比成年患者有着更为重要的临床意义。造成其复发的主要原因可能与其病理结构有密切关系,即多形性腺瘤常为多中心生长,包膜较不完整,且肿瘤常常浸润或突破包膜。
现有研究大部分的关注重点集中于病理相关变量(如:病理亚型、包膜完整性、包膜厚度、伪足、卫星结节、肿瘤大小、肿瘤来源部位、细胞增值相关核抗原及细胞糖蛋白表达等)及手术相关变量(如:切除边界、肿瘤破裂及外渗、术式选择及治疗方法等),且“上述因素均对其术后复发率带来明显影响”这一点已经得到共识。在进行腮腺复发多形性腺瘤的切除手术时,应不同于“单纯剜除术”,选择距离肿瘤边缘0.5~1.0 cm的正常组织内切除肿瘤及部分腺体,可有效防止术后复发。“全腮腺切除术”和“包膜外切除术”的术后复发率最低。所以本病例中,本研究选用的是“包膜外切除术式”。但现有对最佳术式研究的文献多为针对既往临床资料得出的回顾性分析结果,且对于最适合的术式尚未得出一致意见。
研究提出首先根据肿瘤的大小及其在腮腺中的位置划分为4类,接着对于每个类别和各种病理类型,分别提出针对性的手术范围指南。上述完善的分类指南不仅有利于临床多中心前瞻实验进行,且能较为有效地减少不同临床研究中的偏倚,从而利于不同研究间数据的对比整合,更能为临床医师提供更具针对性的指导意见。基于此,未来针对低龄患者人群,也应严格按照上述肿瘤分类选择针对性更强的手术方式。
2.3腮腺多形性腺瘤低龄化给临床诊疗带来的新挑战
基于低龄患者群体的特殊性,腮腺多形性腺瘤低龄化给临床诊疗同样带来其它新的挑战:切口设计时应充分考虑对美观的影响。如本例中,术者选用耳后改良型美容切口,相比于传统的S型切口,对美观的影响更小;早期发现的重要性:低龄患者多处于生长发育期,在进行辅助检查时应优先选择更为安全的常规B超。但研究指出,常规B超检查对于表浅的腮腺良性肿瘤鉴别效果更好,而对于深在的腮腺良性肿瘤,常规B超的效果不及CT检查。
近年来可供低龄患者选择的无创性辅助检查种类日趋丰富。剪波弹性成像技术能有效分辨腮腺内不同实性良性包块的性质,从而可以有效指导临床医师进行鉴别诊断及选择更合理的治疗方式;术后随访对于低龄患者的重要性:术后随访应重点关注腮腺肿瘤的复发可能及术后低龄患者腮腺功能的恢复情况。
综上,腮腺多形性腺瘤低龄患者临床较罕见,且其临床分布及临床表现与高龄患者存在明显差异。早期发现,选择合适的术式及切口,术后随访可有效降低低龄患者的肿瘤复发率。
原始出处:
胡琛,张磊涛,罗醒红,张凯莹.低龄原发腮腺多形性腺瘤:1例报告并文献复习[J].分子影像学杂志,2018,41(01):31-34.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#多形性#
38
#多形性腺瘤#
43
#腮腺#
39
学习了
68
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
71