Sci Rep:iPSC有望治疗遗传性耳聋
2018-02-09 海北 MedSci原创
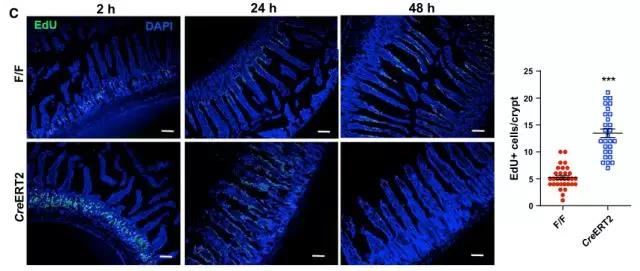
虽然科技发展迅速,但是至今为止,对于遗传性听力损失还不存在任何治愈性的疗法。来自熊本大学的研究人员先前报道了,将野生型CONNEXIN30(CX30)基因转移到CX30缺失小鼠的耳囊中可以帮助其恢复听力。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#遗传性#
37
#遗传性耳聋#
34
#iPS#
30
#PSC#
23
#iPSC#
37
学习了.谢谢!
52
学习谢谢分享
55
非常好.谢谢分享
57
学习了.谢谢分享
62
好好好好好好好好
0