JAMA:对于非囊性纤维化支气管扩张患者 长期用大环内酯类有利有弊 可降低肺部感染加重发生率,但增加耐药率
2013-04-12 高晓方 编译 中国医学论坛报
澳大利亚与荷兰学者的两项研究(即BLESS和BAT研究)表明,在非囊性纤维化支气管扩张患者中,长期使用低剂量大环内酯类(红霉素和阿奇霉素)治疗可降低肺部感染加重发生率,但亦可升高大环内酯类耐药率。论文3月27日发表于《美国医学会杂志》[JAMA 2013,309(12):1251;1260]。 BLESS研究 共纳入117例在过去一年内出现2次及以上感染加重的非囊性纤维化
澳大利亚与荷兰学者的两项研究(即BLESS和BAT研究)表明,在非囊性纤维化支气管扩张患者中,长期使用低剂量大环内酯类(红霉素和阿奇霉素)治疗可降低肺部感染加重发生率,但亦可升高大环内酯类耐药率。论文3月27日发表于《美国医学会杂志》[JAMA 2013,309(12):1251;1260]。
BLESS研究
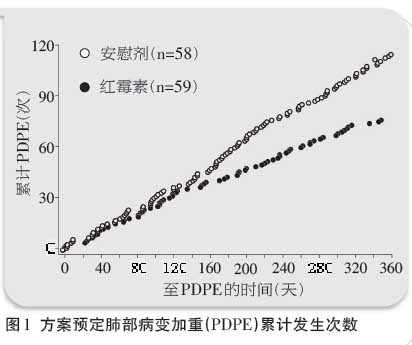
共纳入117例在过去一年内出现2次及以上感染加重的非囊性纤维化支气管扩张患者,并按照1:1比例随机给予为期12个月的琥乙红霉素(400 mg,2次/日)或安慰剂治疗。主要转归为方案预定肺部病变加重(PDPE)的年化平均发生率。

结果为,红霉素可显著降低总体PDPE发生次数[发病率比(IRR)为0.57,图1],并可在基线伴铜绿假单胞菌气道感染的预定亚组人群中降低PDPE发生率(P=0.02)。与安慰剂相比,红霉素可减少24小时咳痰量(P=0.01)并延缓肺功能减退(P=0.04)。红霉素可升高口咽链球菌的大环内酯类耐药率。
BAT研究

共纳入83例在过去一年出现3次及以上下呼吸道感染的非囊性纤维化支气管扩张患者,并随机给予为期12个月的阿奇霉素(250 mg/d)或安慰剂治疗。主要转归为感染加重次数。
结果为,阿奇霉素组和安慰剂组的中位感染加重次数分别为0和2次(P<0.001),至少出现1次加重的患者分别达46%和80%(图2)。在随时间推移的1秒钟用力呼气容积变化方面,阿奇霉素组每3个月升高1.03%,安慰剂组则每3个月降低0.10%。阿奇霉素组和安慰剂组患者的胃肠道不良反应发生率分别为40%和5%;大环内酯类耐药发生率分别为88%和26%。
■ 同期述评
大环内酯类与支气管扩张:以耐药为代价的临床获益
英国贝尔法斯特女王大学 埃尔伯恩(Elborn)
在支气管扩张患者中,感染所致的肺部病情加重对肺功能和健康相关生活质量(QOL)等均有不良影响。上述两项研究证实了EMBRACE研究的结果,后者显示,为期6个月的阿奇霉素治疗可显著降低感染加重频率。
肺部新病原菌出现以及耐药菌增多为抗生素长期维持治疗呼吸疾病的主要隐患。上述研究提示,大环内酯类治疗不会导致新病原菌出现,但对细菌耐药具有显著影响。此外,大环内酯类长期应用可能导致其他抗生素耐药性增加。
研究不足之处在于,研究者仅关注了已知病原菌的抗生素耐药,以及未进行定量培养以明确感染加重率降低是否归因于细菌载量或个体菌种密度降低。
大环内酯类长期治疗对支气管扩张患者的益处须与气道微生物抗生素耐药增多的风险相平衡。此外,大环内酯类亦可能破坏自噬作用,该作用是宿主对非结核分枝杆菌感染作出反应的重要过程。
对临床医师而言,重要的是需要确定哪些患者应使用大环内酯类,以及应使用何种大环内酯类。痰培养、心电图检查以及听力和肝功能测定或可有助于解决上述问题。
与支气管相关的拓展阅读:
- 肺活检增加支气管针吸活检术并发症
- JAMA:大环内酯类抗生素可缓解非囊性纤维化支气管扩张患者的感染性肺病
- Chest:肺活检增加支气管针吸活检术并发症
- JAMA:对于非囊性纤维化支气管扩张患者 长期使用大环内酯类有利有弊
- CHEST:吸入甘露醇或可减少非囊性纤维化支气管扩张患者抗生素使用量 更多信息请点击:有关支气管更多资讯

Effect of Azithromycin Maintenance Treatment on Infectious Exacerbations Among Patients With Non–Cystic Fibrosis Bronchiectasis:
The BAT Randomized Controlled Trial
Importance
Macrolide antibiotics have been shown beneficial in cystic fibrosis (CF) and diffuse panbronchiolitis, and earlier findings also suggest a benefit in non-CF bronchiectasis.
Objective
To determine the efficacy of macrolide maintenance treatment for adults with non-CF bronchiectasis.
Design, Setting, and Participants
The BAT (Bronchiectasis and Long-term Azithromycin Treatment) study, a randomized, double-blind, placebo-controlled trial conducted between April 2008 and September 2010 in 14 hospitals in the Netherlands among 83 outpatients with non-CF bronchiectasis and 3 or more lower respiratory tract infections in the preceding year.
Interventions
Azithromycin (250 mg daily) or placebo for 12 months.
Main Outcome Measures
Number of infectious exacerbations during 12 months of treatment. Secondary end points included lung function, sputum bacteriology, inflammatory markers, adverse effects, symptom scores, and quality of life.
Results
Forty-three participants (52%) received azithromycin and 40 (48%) received placebo and were included in the modified intention-to-treat analysis. At end of study, the median number of exacerbations in the azithromycin group was 0 (interquartile range [IQR], 0-1), compared with 2 (IQR, 1-3) in the placebo group (P < .001). Thirty-two (80%) placebo-treated vs 20 (46%) azithromycin-treated individuals had at least 1 exacerbation (hazard ratio, 0.29 [95% CI, 0.16-0.51]). In a mixed-model analysis, change in forced expiratory volume in the first second of expiration (percent of predicted) over time differed between groups (F1,78.8 = 4.085, P = .047), with an increase of 1.03% per 3 months in the azithromycin group and a decrease of 0.10% per 3 months in the placebo group. Gastrointestinal adverse effects occurred in 40% of patients in the azithromycin group and in 5% in the placebo group (relative risk, 7.44 [95% CI, 0.97-56.88] for abdominal pain and 8.36 [95% CI, 1.10-63.15] for diarrhea) but without need for discontinuation of study treatment. A macrolide resistance rate of 88% was noted in azithromycin-treated individuals, compared with 26% in the placebo group.
Conclusions and Relevance
Among adults with non-CF bronchiectasis, the daily use of azithromycin for 12 months compared with placebo resulted in a lower rate of infectious exacerbations. This could result in better quality of life and might influence survival, although effects on antibiotic resistance need to be considered.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#扩张#
33
#非囊性纤维化支气管扩张#
55
#支气管#
31
#囊性#
37
#发生率#
34
#肺部感染#
36
#大环内酯类#
32