善用他汀,逆转斑块!——如何利用他汀逆转ASCVD患者斑块
2017-08-06 佚名 嘉音
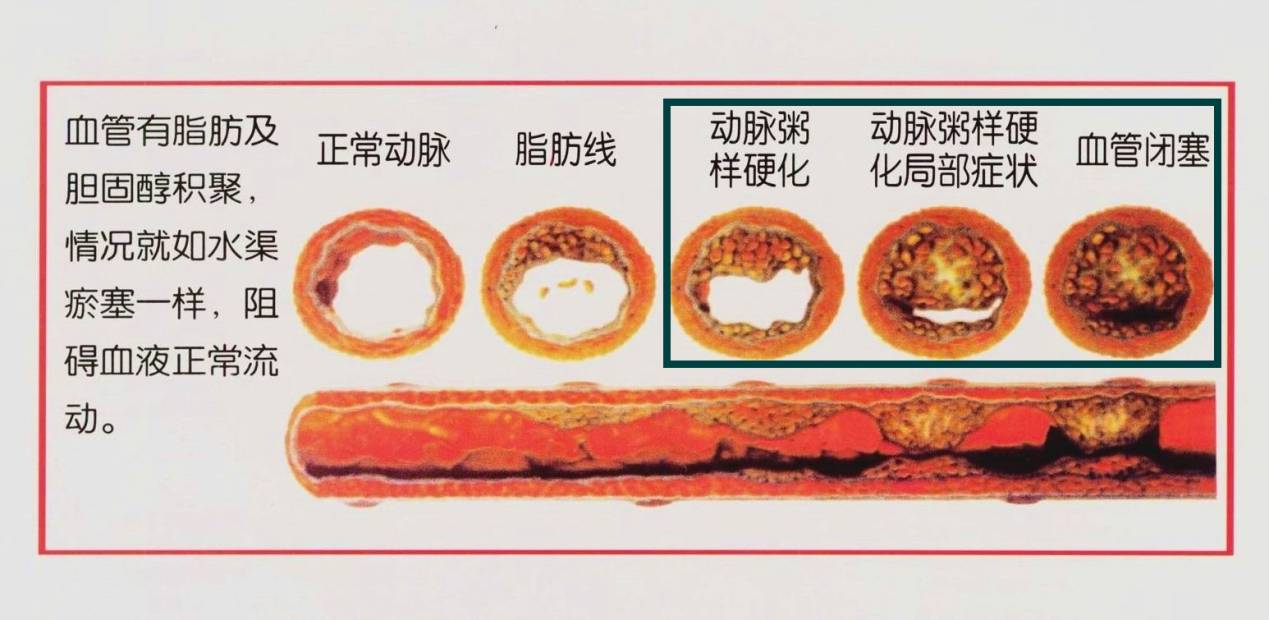
动脉粥样硬化性心血管疾病(atherosclerotic cardiovascular disease,ASCVD )包括冠心病、动脉粥样硬化性卒中和外周血管疾病,病理基础是动脉粥样硬化(AS)。AS是脂代谢紊乱和炎症性血管疾病,随着疾病发展,血管堵塞程度加重,最终可能导致血管彻底阻塞。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASC#
28
善用他汀.逆转斑块!
73
#ASCVD#
49
#斑块#
34
谢谢分享,学习了
73
谢谢分享
72
学习学习
60