NEJM:肝脏棘球绦虫囊肿-病例报道
2018-07-12 xing.T MedSci原创
包虫病是由棘球绦虫引起的。狗是最终的宿主; 当人类或其他动物摄入粪便中的虫卵时,就会传播感染。
患者为一名30岁的男性,因右上腹部间歇性不适15个月而就诊。他住在摩洛哥的一个农村地区,偶尔会和狗接触。
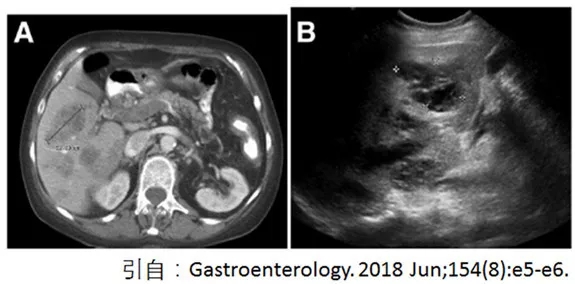
体格检查显示肝肿大,可触及肝脏肿块。实验室检查显示白细胞计数和绝对嗜酸性粒细胞计数正常。腹部超声检查(如图A所示)和计算机断层扫描(如图B所示)发现肝脏右叶有大囊肿,含有包虫膜(如黑色箭头所示)和子囊泡(如白色箭头所示)。酶联免疫吸附试验表明患者血液中的抗棘球蚴IgG抗体指数为16.7(正常值≤11)。
包虫病是由棘球绦虫引起的。狗是最终的宿主; 当人类或其他动物摄入粪便中的虫卵时,就会传播感染。
该患者接受了剖腹手术,在手术期间切除全部囊肿,内容物没有溢出。术后检测到棘球绦虫颗粒体。术后2个月的随访超声检查未见复发迹象。
原始出处:
Ghizlane Lembarki,et al.Echinococcal Cysts in the Liver.N Engl J Med 2018;https://www.nejm.org/doi/full/10.1056/NEJMicm1702005
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#囊肿#
29
#棘球绦虫#
41
#绦虫#
38
学习了.长知识
87
学习谢谢分享
74