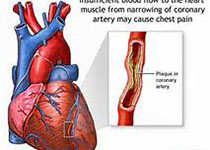
JAHA:急性心梗伴肝硬化患者的β受体阻滞剂该如何选择?
2018-09-30 MedSci MedSci原创
目前,β1选择性抑制剂或非选择性β抑制剂对于肝硬化伴急性心梗的患者是否有效尚不清楚。本研究纳入了台湾NHIRD数据库中的患者,并比较了服用β1选择性抑制剂治疗和非选择性β抑制剂患者的预后,主要终点事件是1年和2年的心血管事件、肝脏不良事件和全因死亡率。最终共纳入了203595名急性心梗患者,其中6355名伴有肝硬化。经过排除标准后,共分析了1769名患者(655名接受β受体阻滞剂治疗,1114名没
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阻滞剂#
31
#受体阻滞剂#
35
#AHA#
41
#β受体阻滞剂#
38
#急性心梗#
32
谢谢!最新的信息读起来就是收获大
58