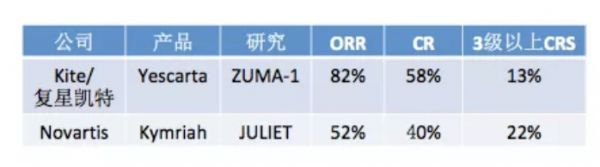
2018 CSCO:朱军教授:全方位解读CAR-T产品在复发难治性淋巴瘤中的应用现状及前景
2018-09-23 Amiee 肿瘤资讯
2018年9月19-21日,第二十一届全国临床肿瘤学大会暨2018年CSCO学术年会在厦门盛大开幕。作为肿瘤领域的一大热点,CAR-T治疗在今年的CSCO会议上关注度只增不减。北京大学肿瘤医院的朱军教授针对CAR-T治疗国内外获批情况及未来应用前景进行了详细介绍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CAR-#
20
#CAR-T产品#
33
#复发难治#
30
希望尽早能在实体瘤上有所突破
56
嗯嗯,学习了。
57
#难治性#
0
了解一下谢谢
68
不错的文章值得拥有哦
61