JCO:西妥昔单抗联合放化疗治疗伴有HIV感染的肛门癌患者的效果有待商榷
2016-12-14 MedSci MedSci原创
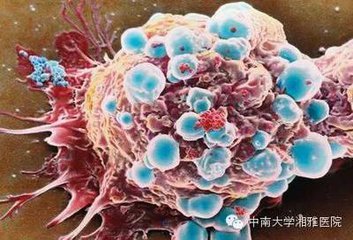
肛管鳞状细胞癌(SCCAC)的产生与肛门生殖器人乳头状瘤病毒相关,并且患者常伴有HIV感染。同时,SCCAC在患者放化疗后常出现高局部缺血(LRF)率。由于西妥昔单抗可以增强人类乳头状瘤病毒引起的口咽SCC放化疗的治疗效果,因此试验旨在探索放化疗SCCAC中使用西妥昔单抗能否减小患者的LRF。
肛管鳞状细胞癌(SCCAC)的产生与肛门生殖器人乳头状瘤病毒相关,并且患者常伴有HIV感染。同时,SCCAC在患者放化疗后常出现高局部缺血(LRF)率。由于西妥昔单抗可以增强人类乳头状瘤病毒引起的口咽SCC放化疗的治疗效果,因此试验旨在探索放化疗SCCAC中使用西妥昔单抗能否减小患者的LRF。
试验共入组45例伴有HIV感染的I-III期的SCCAC患者接受放化疗。治疗方法为:45-54 Gy的放射治疗原发性肿瘤和局部淋巴结,西妥昔单抗每周一次,共8周期。两周期的顺铂合并5-氟尿嘧啶化疗。该试验预计检测3年LRF率至少降低50%,假设历史数据的LRF为35%。
使用预先指定的终点(LRF或活着无LRF且随访<3年)的二项式比例估计,3年LRF率为42%(95%CI,28%-56%;单侧P =0.9),而通过使用与历史数据一致的定义和方法Kaplan-Meier分析的评估为20%(95%CI,10%-37%)。Kaplan-Meier评估的三年PFS为72%(95%CI,56%-84%),OS为79%(95%CI,63%-89%),4级毒性发生率为26%,与治疗相关死亡率为4%。
试验结果可以看出,伴有HIV的SCCAC患者的确需要放化疗,虽然使用西妥昔单抗可以减少患者的LRF发生率,但是20%的复发率和26%的4级毒性发生率表明患者继续治疗需要采用更为有效和毒性更小的方案。
原始出处:Sparano JA, Lee JY, Palefsky J, Henry DH, Wachsman W, Rajdev L, et al. Cetuximab Plus Chemoradiotherapy for HIV-Associated Anal Carcinoma: A Phase II AIDS Malignancy Consortium Trial. Journal of Clinical Oncology 2016:JCO.2016.69.1642.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肛门#
29
#JCO#
26
#西妥昔#
25
谢谢分享,学习了
90
#放化疗#
33