【一般资料】
患者37岁,G4P1,
【主诉】
因“双侧输卵管切除术后2年,要求生育二胎”就诊。
【现病史】
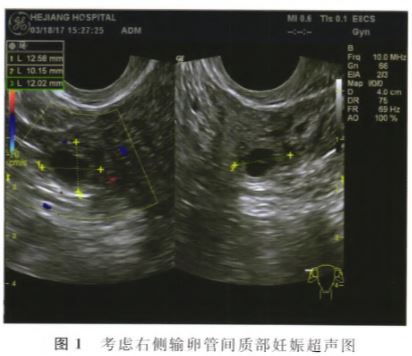
者平素月经规律,经期7d,周期28d,经量中等,无痛经。性生活正常。2007年足月剖宫产1子,现体健。2010年12月因右侧输卵管妊娠于杭州市一医院行腹腔镜下右侧输卵管切除术;2014年因左侧输卵管妊娠在浙江大学附属妇产科医院行腹腔镜下左侧输卵管切除术。2015年3月至2016年7月在外院多次自然周期取卵均无优质胚胎。2016年8月查抗苗勒氏管激素(AMH)0.04ng/ml。2016年12月我院促排卵治疗后取卵,经体外培养获得第3天优质胚胎1枚。8细胞2级胚胎含8%碎片(8-8%一2);2017年2月17日行激素替代治疗(HRT)周期后冻融胚胎移植(FET)1枚胚胎,移植后常规黄体支持,移植后12d查血G—HCG111.7U/I。,之后多次复查血HCG上升缓慢;移植术后一直无下腹部疼痛,无阴道出血。2017年3月16日查血13-HCG2575.1U/I。;3月18日经阴道B超提示:前位子宫,大小正常,肌层回声均匀,双层内膜厚约1.1cm,宫内未见明显异常回声;双侧卵巢可及;子宫右侧角部可见环状混合回声,大小约1.3ClTIx1.0cm×1.2cm,内见暗区,暗区内见卵黄囊样回声;盆腔内未见明显游离积液(见图1)。考虑右侧输卵管残端间质部妊娠。3月19日以“疑似宫外孕”收住院。外阴已婚型,阴道通畅,宫颈光滑,无摇举痛;宫体:前位,大小正常,质软,活动,无压痛,右附件区轻压痛,未触及包块,左附件区未触及明显异常。
【初步诊断】
(1)疑似宫外孕;(2)双侧输卵管切除术后。
【体格检查】
入院后完善术前相关检查,体温(T)37.4。C,心率(P)81次/min,呼吸(R)18次/min,血压(BP)109/63mmHg。患者一般状态良好,神志清楚,自主体位,查体:心肺无异常,腹部平软,压痛、反跳痛及肌紧张阴性,腹部无移动性浊音。
【治疗】
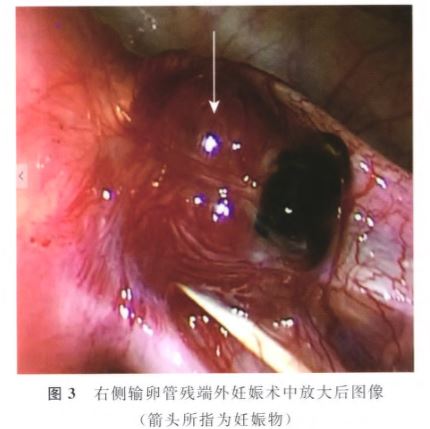
积极完善相关术前检查,于3月20日急诊行腹腔镜探查术,术中见:子宫前位,正常大小,表面光滑;双侧输卵管间质部以远缺如,双侧卵巢体积明显小,表面皱缩,右侧宫角外原输卵管残端外可见一直径约1.5cm血性包块,表面布满增生的毛细血管(图2和图3箭头所指);道格拉斯窝存在,盆腔内未见游离液体,盆腹腔余脏器未见明显异常。行盆腔妊娠物切除术:双极电凝钳分别钳夹、电凝、切断妊娠物的基底部及周围的毛细血管样组织,完整切除妊娠物,袋装后完整取出,取出的组织送常规病理。手术过程顺利,术后给予常规抗感染、输液等对症支持治疗。术后诊断:(1)异位妊娠(右侧输卵管残端外妊娠);(2)双侧输卵管切除术后。术后第2天复查血G—HCG777.4U/L。术后病理提示:“盆腔妊娠物”可见绒毛组织,符合妊娠物(图4)。术后第3天患者体温正常,切口愈合好,出院。


【讨论】
ART是治疗不孕症的重要手段,IVF—ET是ART最主要的治疗方法之一。双侧输卵管不通或切除是IVF—ET最常见的一种适应症。在治疗不孕症的同时,ART也增加了EP的发生风险。输卵管炎症、阻塞或积水以及宫外孕术后等行IVF—ET助孕,EP发生率明显上升。诸多研究对自然妊娠和ART妊娠的临床结局分析发现,ART过程中EP的发生率比自然妊娠增加了2~5倍,ART助孕周期中EP的发生率可高达2%~8%,且EP的类型呈现复杂化的趋势,有一些EP发生在自然妊娠中少见甚至一般认为不可能发生的位置。行腹腔镜下输卵管切除术后的患者,其输卵管残端妊娠的发生率不断升高,国内诸多文献报道过类似病例的发生。甚至万琪等曾报道过1例患者6次EP。本病例是双侧输卵管切除术后,右侧输卵管残端外妊娠。查阅国内外相关文献,类似报道较少,国内孙燕茹等凹曾报道腹腔镜治疗双侧输卵管切除术后腹膜后妊娠1例。
1.病因及发病机制:
IVF助孕技术中EP发生率较自然妊娠发生率高。有EP史的患者,IVF-ET后再次发生EP的几率明显高于对照组。输卵管切除术后,输卵管间质部未遭到破坏,或管腔未闭。行腹腔镜操作时,一般使用双极电凝后切除患侧输卵管,其原理是双极高频电流可引起局部组织内碳化,实际操作中当输卵管周围组织被碳化到一定程度时,电凝过程就全部结束,容易导致输卵管未达到全部碳化,容易形成输卵管残端瘘;妊娠过程中卵母细胞则可能通过受精并着床于残留输卵管残端;或IVF—ET后胚胎通过输卵管残端瘘种植在输卵管残端外或盆腔。有研究证实,胚胎移植操作过程中移植管内的液体量、移植管植入宫腔的深度、胚胎注入时的力度和速度等都可能影响胚胎的移动。如移植管内液体量过多(>30肚1)、移植管进入宫腔的深度过深,或因移植困难进行反复操作等,都可能引起子宫内膜受损以及子宫收缩,可能导致移植的胚胎被挤人输卵管,导致EP的发生。另外,体内高雌、孕激素水平,促排卵时大量使用外源性促性腺激素等都可能影响输卵管的正常蠕动,继而影响胚胎的正常运行,导致EP发生。
2.诊断及治疗:
虽然有既往双侧输卵管切除的病史,胚胎移植后血B—HCG升高缓慢并不是EP的特异性指标,腹痛和阴道出血也不具有特异性,因此该病例EP的诊断最终是通过阴道B超检查。血J3一HCG升高,B超提示:宫内未见妊娠囊样回声,宫外尤其卵巢外见不均质回声团或混合性回声团,当彩超提示该回声团血流丰富时则高度怀疑EP的可能。临床上行IVF助孕治疗时,为保证移植的成功率,有时会选择移植2个胚胎,对于部分患者由于客观因素可能会选择移植3个胚胎。因此,生殖医学科的B超医生在临床上作中应具有风险意识,尤其在对移植多个胚胎的患者进行B超检查时,在确认宫内孕囊存在后,应进一步探查双侧附件区,以便及时发现宫内外复合妊娠及多部位的复杂EP的可能。
3.预防:
双侧输卵管切除术后,患者若有生育要求,均会选择IVF—ET助孕。为避免输卵管切除术后输卵管残端EP的发生,医生在对患者行输卵管切除时需注意以下几点:尽量靠近输卵管凝切,以保留尽量多的卵巢血供,即尽量减少对卵巢功能的影响;保留输卵管的残端要短,以免发生输卵管残端妊娠;输卵管切除时残留输卵管越长,发生再次EP可能性越大。万琪等口3报道的病例中,左侧输卵管妊娠1次,其余5次均为右侧输卵管妊娠,其中5次右侧输卵管妊娠,除1次保守治疗外,其余4次均行病灶切除术,仅最后1次手术时同时行双侧输卵管近端结扎术。输卵管切除后对输卵管残端(间质部)进行缝合或单极电凝钩或双极电凝钳额外电凝,进一步破坏残留的间质部,使残留的间质部管腔闭合,同时用2-0可吸收线“8”字缝合输卵管残端,防止输卵管残端瘘的发生。殷宝莉等研究发现,冻融胚胎单囊胚移植可以有效降低EP的发生,尤其是对于反复种植失败和有EP病史的患者。这可能与以下因素有关:(1)选择冷冻周期可以有效避免新鲜周期中明显高于生理水平的雌激素、孕激素环境;(2)囊胚移植更接近于生理状态;(3)囊胚的体积较大,相对卵裂期胚胎而言囊胚更难向输卵管逆行,因此可以有效降低EP的发生风险,改善临床妊娠结局。陈欢欢等L1列研究证实,间苯三酚应用于ART辅助治疗时,可以有效减少对子宫内膜的刺激,抑制子宫平滑肌痉挛性收缩,减少子宫内膜负向蠕动波。因此,建议胚胎移植选择有经验的移植医生(移植医生相对固定),在进行胚胎移植操作前注射宫缩抑制剂(问苯三酚、阿托西班等),胚胎移植时移植管外壳探官腔时装上内芯(即移植管),且内芯超出外壳2~3mm,患者适当充盈膀胱,在腹部超声引导下进行,可明显改善前位子宫的曲度,减轻移植的困难程度,避免了反复操作对子宫的刺激继而导致宫缩,造成子宫内膜的损伤、出血,当外壳通过宫颈内口后即停止、固定外壳,用内芯继续进入宫腔1cm左右,腹部超声下看内芯进人是否顺利,若内芯进入顺利,则撤出内芯,由实验室人员装好事先准备好的胚胎,将胚胎移植管缓慢送至距离宫腔底部1.5cm左右处或宫腔内膜最厚处,固定内芯,轻轻撤出外壳,缓慢推出胚胎,静静停留数秒,内芯和外壳一起轻轻退出,实验室认真检查移植管,以判断胚胎是否被带出,术后患者静卧1~2h,常规黄体支持。综上,对IVF—ET术后妊娠的患者,若血BHCG早期上升缓慢,建议B超检查应相对提前,以明确宫内妊娠孕囊数及胚芽及原始心管搏动情况,并要认真排查双侧附件区有无异常情况,尤其对移植多个胚胎、既往有EP史、盆腔手术史、宫内未见明显孕囊或宫内孕囊数少于移植胚胎数的患者。对于超声提示EP可能、血HCG较高、附件区包块较大者建议尽早进行腹腔镜探查以明确诊断、去除病灶。
原始出处:
吴瑞芳. 双侧输卵管切除术后输卵管残端外异位妊娠1例及文献复习[J]. 生殖医学杂志 2018年第03期
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#输卵管切除术#
36
#输卵管#
0
#切除术#
36
#异位妊娠#
39
#双侧#
33
阅
59
学习
69