Blood:来那度胺联合obinutuzumab用于复发性/难治性滤泡性B细胞淋巴瘤的安全性和疗效
2018-08-03 MedSci MedSci原创
中心点:口服来那度胺联合obinutuzumab用于复发性或难治性滤泡性B细胞淋巴瘤(FL)患者耐受性好、疗效客观。来那度胺与obinutuzumab(1000mg)联合应用时的推荐剂量为20mg。摘要:Obinutuzumab是II型抗CD20单克隆抗体,比利妥昔单抗更能增强抗体依赖性的细胞毒性。考虑到来那度胺与利妥昔单抗联合应用的疗效,现Franck Morschhauser等人开展一1b期研
口服来那度胺联合obinutuzumab用于复发性或难治性滤泡性B细胞淋巴瘤(FL)患者耐受性好、疗效客观。
来那度胺与obinutuzumab(1000mg)联合应用时的推荐剂量为20mg。
摘要:
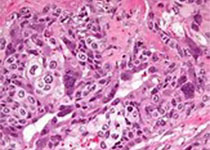
Obinutuzumab是II型抗CD20单克隆抗体,比利妥昔单抗更能增强抗体依赖性的细胞毒性。考虑到来那度胺与利妥昔单抗联合应用的疗效,现Franck Morschhauser等人开展一1b期研究,评估来那度胺与obinutuzumab联合(GALEN)应用的安全性和疗效。
研究人员招募年满18岁的进行过利妥昔单抗治疗的复发性或难治性FL患者,予以口服来那度胺,按剂量递增疗法(10mg[7人]、15mg[3人]、20mg[6人]、25mg[3人]),28天一疗程,第1疗程的第1-21天、第2-6疗程的2-22天用药。Obinutuzumab 1000mg IV,第1疗程的第8、15和22天以及第2-6疗程的第1天用药。
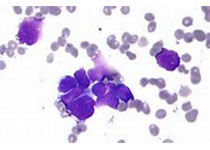
在第1疗程根据剂量限制性毒性(DLT)以3+3的模式增加剂量,来确定最大耐受剂量(MTD)。研究期间,共发生164例副反应事件(AEs),其中139例为1-2级。最常见的AEs有便秘(52.6%)、中性粒细胞减少(47.4%)和乏力(36.8%);3-4级AEs有14例,其中9例(64.3%)为中性粒细胞减少,但无发热性中性粒细胞减少。2位患者出现4次DLTs,均判定与治疗无关。未达到最大耐受剂量。12位(63.2%)患者获得缓解:8位完全缓解、3位未明确是否是完全缓解、1位部分缓解。
口服来那度胺联合obinutuzumab治疗复发性或难治性滤泡性淋巴瘤,耐受性良好,疗效可观。根据第2疗程发生3-4级中性粒细胞减少的风险,推荐来那度胺的剂量为20mg。
原始出处:
Franck Morschhauser,et al.An open-label, phase Ib study of obinutuzumab plus lenalidomide in relapsed/refractory follicular B-cell lymphoma. Blood 2018 :blood-2018-05-853499; doi: https://doi.org/10.1182/blood-2018-05-853499
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
36
#细胞淋巴瘤#
34
#复发性#
27
#B细胞#
25
#Obinutuzumab#
36
#难治性#
27
谢谢梅斯提供这么好的信息,学到很多
50