Hypertension:PPI对先兆子痫的影响!
2017-01-24 xing.T MedSci原创
PPIs可以降低sFlt-1和可溶性内皮因子的分泌,减轻血管内皮功能障碍,血管扩张,降低血压,并具有抗氧化和抗炎的特性。他们对于先兆子痫等其他内皮功能障碍参与的疾病具有潜在的治疗价值。
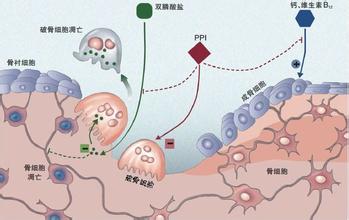
先兆子痫是妊娠期的严重并发症,从胎盘中分泌出过量的抗血管生成因子可溶性fms样酪氨酸激酶-1(sFlt-1)和可溶性内皮因子,可导致高血压、血管内皮功能障碍以及多器官损伤。氧化应激和血管炎症可以加重血管内皮损伤。可以阻断这些病理生理过程的药物将是一个具有吸引力的治疗选择。怀孕期间服用质子泵抑制剂(PPI)治疗胃食管反流是安全的。
近日,心血管权威杂志Hypertension上发表一篇研究文章,研究人员对主要的人体组织和动物模型进行了一项功能研究来评估PPIs对sFlt-1和可溶性内皮因子分泌/血管扩张、血压和血管内皮功能的效应。
质子泵抑制剂可以降低胎盘滋养层细胞、先兆子痫孕妇的胎盘外植体和内皮细胞分泌的sFlt-1和可溶性内皮因子,并且还可以减轻肿瘤坏死因子α诱导的血管内皮功能障碍:质子泵抑制剂阻断血管内皮细胞粘附分子-1的表达,白细胞粘附于内皮上,并阻断内皮管形成。质子泵抑制剂降低内皮素-1的分泌和增强内皮细胞迁移。有趣的是,PPI埃索美拉唑可以使早产先兆子痫孕妇和正常妊娠孕妇母体血管舒张,并且当剥除内皮后这一效应消失。埃索美拉唑降低在胎盘中过表达人类sFlt-1的转基因小鼠模型血压。质子泵抑制剂可以上调内源性抗氧化防御和降低从胎盘组织及内皮细胞分泌的细胞因子。
研究人员发现,PPIs可以降低sFlt-1和可溶性内皮因子的分泌,减轻血管内皮功能障碍,血管扩张,降低血压,并具有抗氧化和抗炎的特性。他们对于先兆子痫等其他内皮功能障碍参与的疾病具有潜在的治疗价值。
原始出处:
Kenji Onda, et al. Proton Pump Inhibitors Decrease Soluble fms-Like Tyrosine Kinase-1 and Soluble Endoglin Secretion, Decrease Hypertension, and Rescue Endothelial Dysfunction. Hypertension. 2017. http://hyper.ahajournals.org/content/early/2017/01/23/HYPERTENSIONAHA.116.08408
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
28
#TENS#
31
PPIs可以降低sFlt-1和可溶性内皮因子的分泌,减轻血管内皮功能障碍,血管扩张,降低血压,并具有抗氧化和抗炎的特性。
67
学习,感谢分享
53
长见识了
65
啊
68
继续学习中
69
#Hypertension#
34
很好的学习资料,感谢!
18
很好的学习资料,感谢!
18