本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

国际骨质疏松基金会(IOF)发布的一项题为“男性骨质疏松症:缘何需要改变”的最新报告显示,三分之一的髋部骨折发生于男性,骨折后1年内死亡率高达37%,提示亟需加强对男性骨质疏松问题的重视。 研究者澳大利亚内分泌学会主席兼澳大利亚蒙纳士大学的Peter Ebeling及其同事对2011年东欧及中亚地区骨质疏松症审计文件及2013年亚太地区骨质疏松症审计文件的回顾显示,目前男性骨质
患者男,33岁,跑马拉松后六周,出现左髋疼痛。 比赛前三周患者就出现了首次髋部疼痛 。二十英里的比赛,让患者痛苦不堪。 最初他被诊断为股四头肌劳损,接受理疗。 六周后的影像学检查显示亚急性、移位的股骨颈骨折,如下图所示。并且磁共振成像也证实了骨折。 如果不能及早识别骨折,错过治疗时期,这些损伤会导致股骨头坏死,就需要进行髋关节置换了。 本案例也告诫我们,
一项新研究披露,进食含有大量水果、蔬菜、鱼类、坚果、豆类和全谷类的地中海饮食似乎与女性髋部骨折风险的降低相关,尽管其实际的风险降福颇小。 骨质疏松性骨折是老龄化社会医疗保健系统的一个主要负担。有关摄取与骨代谢有关的营养素是否能防止骨折的研究结果一直不甚一致。 德国巴伐利亚州维尔茨堡大学的Bernhard Haring,M.D.,M.P.H.和共同作者对因
董纪元 董纪元,解放军总医院主任医师、教授,亚洲骨科人工关节学会委员,华裔骨科学会关节外科分会理事 35岁的李先生是一名项目经理,天天忙着出差、应酬,经常为了一个项目与客户喝上十顿八顿酒。去年开始,他老觉得腿疼,但症状时轻时重,他以为是太过劳累导致的,就没当回事儿。可这半年来越发严重,去医院经检查发现,他患上了双侧股骨头坏死。 酒在中国的社交中担负着重要角色,商务活动、家
据6月25日刊《美国医学会杂志》上的一则研究披露,在2004年至2011年间接受髋关节修复术的5万6000多名成年人中,与全身麻醉相比,使用局部麻醉与术后30天时死亡风险的下降没有关系,但与住院时间的适度缩短有关。 每年,美国会发生30多万起的髋骨骨折,它会导致功能性能力丧失和死亡。根据文章的背景资料,在做髋部骨折手术时使用局部麻醉可减少手术后并发症,而手术指南呼吁更广泛地用局部麻醉来进行髋部骨
美国一项研究显示,在疗养院居住的髋部骨折患者中,特别是接受非手术治疗、年龄较长的老年人和有多种并发症及认知障碍的患者的生存率和活动功能均较低。因此,应将结果相关的预后信息加入此群体的护理计划中。研究6月23日在线发表于《美国医学会杂志·内科学》(JAMA Intern Med)。 此项回顾性队列研究纳入了自2005年7月至2009年6月,髋部骨折住院治疗后在疗养院护理的60111例


梅斯医学MedSci APP
医路相伴,成就大医
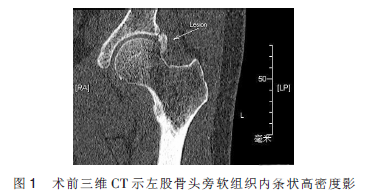
#钙化性肌腱炎#
26
受教.
57
#髋部#
0
#肌腱炎#
30
#肌腱#
32
#钙化性#
26