SCI REP:术前NLR与肿瘤相关因素可预测NF-PNET患者的淋巴结转移!
2017-12-13 xing.T MedSci原创
NLR、症状性诊断、肿瘤大小与淋巴结转移有关。这些结果表明术前NLR ≥1.80,肿瘤大小超过2.5cm 和症状性诊断与接受切除手术的NF-PNETs患者淋巴结转移独立相关。
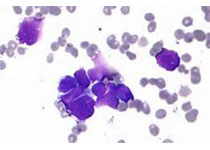
淋巴结(LN)状态对胰腺神经内分泌肿瘤(PNETs)患者的生存是非常重要的。因此,对LN转移相关因素的研究具有重要的临床意义。
近日,Scientific reports杂志上发表了一篇研究文章,研究人员的目的是评估术前中性粒细胞与淋巴细胞比率(NLR)、血小板与淋巴细胞比率(PLR)以及可能的临床参数在无功能性PNETs(NF-PNETs)患者淋巴结转移中的预测价值。
研究人员回顾性审查了101例接受根治性切除和淋巴结清扫术的NF-PNET患者。研究人员确定了临床病理因素与LN转移及预后之间的关系。
研究人员发现二十七例(26.7%)患者有淋巴结转移。淋巴结转移与无疾病生存率独立相关(P=0.009)。根据接受者操作特征曲线,NLR、PLR以及肿瘤大小预测淋巴结转移的理想临界值分别为1.80、168.25和2.5cm。在多变量分析中,NLR(P=0.017)、症状性诊断(P=0.028)、肿瘤大小(P=0.020)与淋巴结转移有关。这些结果表明术前NLR ≥1.80,肿瘤大小超过2.5cm 和症状性诊断与接受切除手术的NF-PNETs患者淋巴结转移独立相关。
由此可见,这些结果有助于手术前进一步规划淋巴结切除术。
原始出处:
Bo Zhou,et al. Preoperative neutrophil-to-lymphocyte ratio and tumor-related factors to predict lymph node metastasis in nonfunctioning pancreatic neuroendocrine tumors.Scientific reports. 2017. https://www.nature.com/articles/s41598-017-17885-y
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#NET#
32
#肿瘤相关因素#
21
学习学习学习
66
#淋巴结#
22
#淋巴结转移#
32
#NLR#
40
#相关因素#
22
学习学习
57
谢谢分享.学习了
43
谢谢分享.阅读
58