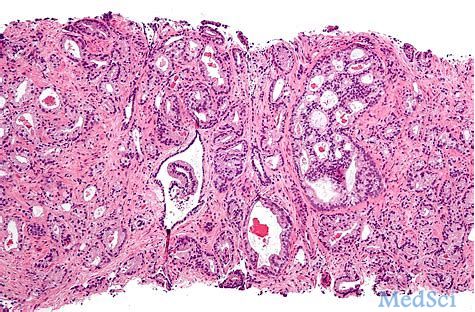
Prostate Cancer P D:前列腺癌患者前列腺切除术后男性的死亡日期和死因调查
2019-05-10 AlexYang MedSci原创
国家死亡指数(NDI)是一个集中式的数据库,包含了死亡证明相关信息,这些信息被健康和医疗调查人员用来参考确定人口动态统计情况。然而,该数据库经常包含错误的死因。由于NDI依赖于前列腺癌(PC)患者根治性前列腺切除(RP)相关研究的治疗结果数据,最近,有研究人员通过参考SEARCH数据库的死亡数据来确定NDI数据的可靠性。研究发现,在SEARCH中共有1312名男性死亡,然而,NDI却报道这些男性的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
30
#Prostate Ca#
36
#前列腺切除#
32
#ROS#
28
#PRO#
30
学习了谢谢分享
81
前列腺癌相关研究,学习了,谢谢梅斯
47