Intens Care Med:术后腹腔感染重症患者的抗生素使用越久越好? NO!
2018-06-13 甘文思 SIFIC感染官微
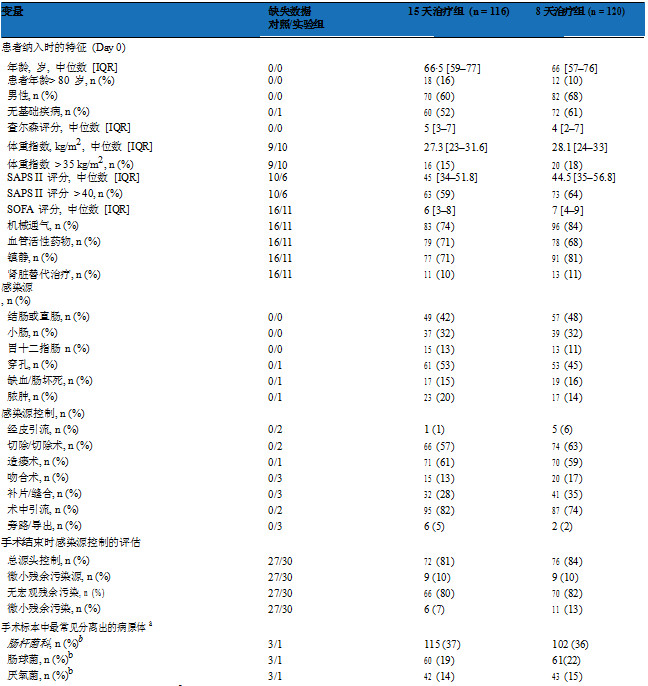
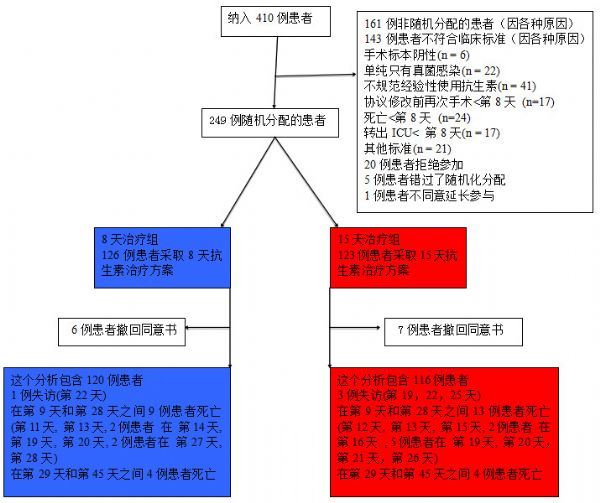
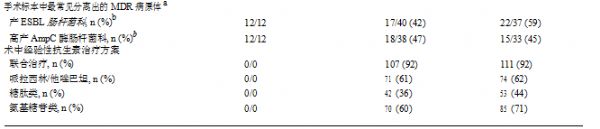
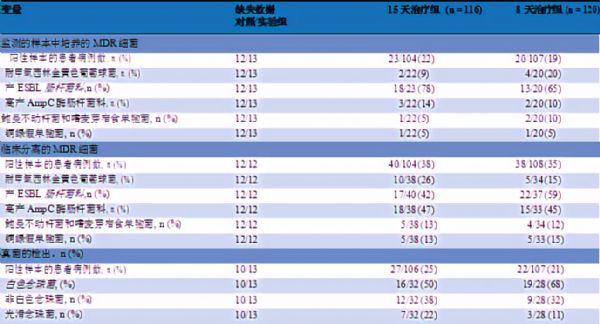
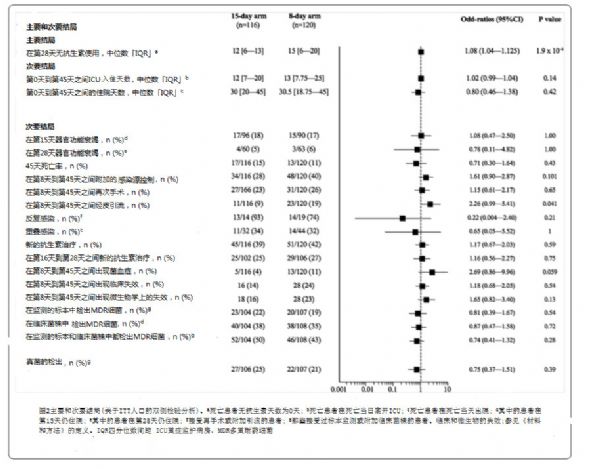
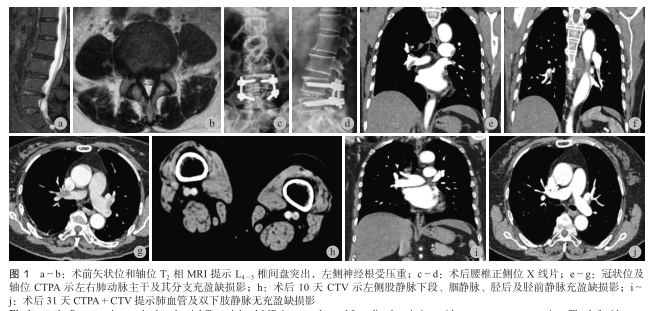
减少抗生素治疗的持续时间是抗菌药物管理的一项基本措施。对于复杂的腹腔感染,抗生素治疗的最佳持续时间已经被广泛讨论,但对于ICU患者缺乏相关的数据。现有的指导方针没有提供相关的建议,只是建议决策过程应该基于临床医生的判断和实验室结果。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不错,学习了
75
#抗生素使用#
37
#腹腔感染#
41
#TENS#
37
#重症患者#
29
#Med#
28
学习了
67
学习谢谢分享
53
不错学习了很有用
43
学习学习.了解了解
49