Cell Research:生命中心董晨研究组发现肿瘤免疫治疗新靶点
2017-07-10 生命联合中心 生命联合中心
2017年7月,生命中心董晨研究组在《Cell Research》杂志在线发表题为“Inhibition of the B7-H3 immune checkpoint limitstumor growth by enhancing cytotoxic lymphocyte function”的研究论文,揭示了免疫检查点B7-H3在抗肿瘤免疫反应中的负调控作用、其作用机制及其潜在的临床应用前景。
2017年7月,生命中心董晨研究组在《Cell Research》杂志在线发表题为“Inhibition of the B7-H3 immune checkpoint limitstumor growth by enhancing cytotoxic lymphocyte function”的研究论文,揭示了免疫检查点B7-H3在抗肿瘤免疫反应中的负调控作用、其作用机制及其潜在的临床应用前景。
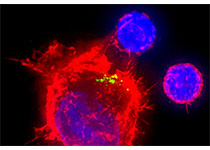
人体内的免疫效应细胞(如CD8+ T淋巴细胞和NK细胞——自然杀伤细胞)可以识别并杀伤癌细胞,但它们的杀伤功能往往被它们激活后上调的免疫检查点分子(如PD-1、CTLA-4和Tim-3)所抑制。拮抗免疫检查点的药物(如PD-1、CTLA-4中和抗体)在多种癌症的临床试验中有突出的疗效并已获美国FDA批准用于黑色素瘤、非小细胞肺癌等疾病的治疗。但只有一小部分的病人在用药后可以产生较好的应答,另外一大部分病人在短暂应答之后癌症继续恶化,这提示我们可能还有其它免疫检查点分子参与抵御免疫杀伤,也可以作为肿瘤免疫治疗或联合治疗的药物靶点。B7-H3是B7蛋白家族的一员,与PD-L1(PD-1的配体)有28%的序列同源性,董晨等研究组之前研究表明B7-H3调控T细胞活化,它在肿瘤组织中的表达与疾病进展和预后相关。然而,B7-H3在抗肿瘤免疫应答中的功能和作用机制尚未研究清楚,B7-H3的受体也未确定。
董晨研究组发现B7-H3在人类肿瘤都普遍高表达,并在肿瘤病人(黑色素瘤、肝癌)和荷瘤小鼠中检测B7-H3及其受体的表达。B7-H3高表达于肿瘤组织中的抗原呈递细胞(如巨噬细胞、树突状细胞)和肿瘤细胞表面,而它的受体则主要在CD8+ T和NK细胞上表达,说明肿瘤微环境中B7-H3及其受体的相互作用有可能抑制抗肿瘤免疫效应细胞的功能。接着,他们在多个小鼠肿瘤模型中探究敲除B7-H3基因或注射B7-H3中和抗体对肿瘤生长的影响。当B7-H3信号通路被抑制时,皮下注射的E.G7、A20淋巴瘤、MOPC315骨髓瘤的生长减缓,静脉注射的B16黑色素瘤的肺转移癌灶也减少,而且这种抑制肿瘤的效应依赖于CD8+ T和NK细胞。
于是,董晨研究组进一步探讨B7-H3如何影响肿瘤微环境中CD8+ T和NK细胞的功能。虽然在B7-H3敲除小鼠(E.G7模型)中肿瘤浸润的CD8+ T的比例没有变化,但肿瘤抗原(OVA)特异性CD8+ T细胞的比例上升;同时,B7-H3敲除小鼠肿瘤中的CD8+ T细胞分泌gamma干扰素和颗粒酶B等杀伤肿瘤的效应分子增多,表明B7-H3抑制抗肿瘤CD8+ T细胞的增殖和效应功能。另外,B7-H3敲除小鼠(E.G7及B6-F10模型)中NK细胞的数量和杀伤功能显着上调;与缺失B7-H3的树突状细胞共培养的NK细胞对靶细胞具有更强的杀伤效应;体外ADCC实验表明,B7-H3蛋白可直接作用于人NK细胞来抑制其去颗粒过程。
由于抑制B7-H3信号后肿瘤中的CD8+ T和NK细胞表面的PD-1上调,而且E.G7荷瘤小鼠的肿瘤组织中同时表达B7-H3和PD-L1,董晨研究组进一步探究抗B7-H3和PD-1中和抗体联合用药的可能性。在E.G7小鼠模型中,注射肿瘤7天后B7-H3抗体和PD-1抗体的联合治疗相比于单独治疗可以更好地抑制肿瘤生长;但如果在肿瘤生长早期(第三天)就开始注射抗体则观察不到协同作用。他们的研究表明,B7-H3抗体与PD-1抗体的联合用药有望进一步改善目前用于临床的PD-1抗体治疗的疗效,尤其是对于晚期肿瘤。
董晨教授为本文的通讯作者,董晨研究组前博士后Young-hee Lee和Natalia Martin-Orozco为本文的共同第一作者,论文的其它作者还包括来自清华大学、美国安德森癌症研究中心、美国国立儿童医院、多伦多大学和苏州鑫康合公司等多个单位的研究者。
原始出处:
Young-hee Lee, Natalia Martin-Orozco, et al. Inhibition of the B7-H3 immune checkpoint limits tumor growth by enhancing cytotoxic lymphocyte function. Cell Research advance online publication 7 July 2017;doi: 10.1038/cr.2017.90
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
27
#Cell#
25
#新靶点#
25
#治疗新靶点#
29
#Research#
29
肿瘤微环境之间,肿瘤微环境与肿瘤之间的作用网络应该很复杂。
33
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
42
生命中心董晨研究组发现肿瘤免疫治疗新靶点
43
学习了,不错啊
48
不错的,学习了,谢谢分享!
50