行医经验:肘关节损伤治疗之我见
2016-05-07 暂不知 请告知 中国骨与关节杂志
笔者在2015COA大会上作了关于“肘关节损伤治疗进展”的报告,应《中国骨与关节杂志》之邀,撰写一篇相关述评。目前国内在肘关节方面的认识和治疗水平已有了很大的提高,但临床上肘部创伤的总体治疗效果仍不令人满意,仍是治疗难点之一。治疗后出现内固定失效、骨折不愈合、关节对合异常及肘和前臂功能障碍仍十分常见。笔者现就肱骨髁间骨折、全肘关节置换、肘关节复杂骨折脱位和肘关节僵硬松解术这四个热点谈谈肘部创伤
笔者在2015COA大会上作了关于“肘关节损伤治疗进展”的报告,应《中国骨与关节杂志》之邀,撰写一篇相关述评。目前国内在肘关节方面的认识和治疗水平已有了很大的提高,但临床上肘部创伤的总体治疗效果仍不令人满意,仍是治疗难点之一。治疗后出现内固定失效、骨折不愈合、关节对合异常及肘和前臂功能障碍仍十分常见。笔者现就肱骨髁间骨折、全肘关节置换、肘关节复杂骨折脱位和肘关节僵硬松解术这四个热点谈谈肘部创伤的治疗现状和笔者的体会。
肱骨髁间骨折
一直以来,肱骨髁间骨折都被认为是“很难处理的少数几个骨折之一”。数十年来随着手术技术的进步和内固定器械的改进,其疗效有了明显改善,但仍欠满意,优良率为60%~80%,且并发症较多,包括内固定失效、骨折不愈合或畸形愈合、异位骨化、肘僵硬、尺神经炎等。在肱骨髁间骨折的治疗方面,尚有争议。
手术入路的选择:充分的手术显露对关节面的解剖复位和有效内固定十分重要。手术时一般取后正中入路,目前关于是否行鹰嘴截骨存在一定的争议,许多学者建议从肱三头肌两侧入路或劈肱三头肌腱进行显露,但笔者仍认为绝大多数肱骨远端骨折的最佳手术入路是经鹰嘴截骨入路。通常建议在尺骨近端关节面的裸区进行V型鹰嘴截骨。开始时使用摆锯进行截骨,并使用骨刀完成最终截骨,以在截骨部位形成不规则断端、减少骨量丢失、避免关节软骨破坏。肱三头肌两侧入路或劈肱三头肌腱适用于较简单的骨折,若需要在术中再决定是进行内固定还是关节置换,采用这一入路就很有好处,但显露相对局限,且一旦肱三头肌愈合出现问题可引起伸肘无力。
肱骨髁间骨折的固定方式:AO组织提出了经典的垂直钢板固定方法并获得了广泛应用,即:1枚或2枚螺钉固定关节面骨块,再用2块垂直钢板固定:1块固定在后外侧,另1块固定在内侧。Diedefichs等研究发现肱骨小头松质骨骨密度及骨皮质厚度均最低,双钢板垂直放置时远端外侧骨折块仅由1枚或2枚短螺钉固定,而肘关节在日常生活中经常承受内翻应力,因此外侧柱固定欠牢靠,远端骨折块固定至肱骨干也不稳定,易出现髁上水平的骨折不愈合或因长时间制动而导致关节僵硬。Sanchez-Sotelo等提出采用平行钢板技术,将两块钢板分别放置在内、外侧柱的侧方固定,他们认为这种固定方式对远端关节面的支撑更佳,且可以更好地进行髁上部位的加压。很多生物力学试验也证实了平行钢板的力学强度优于垂直钢板,但在临床上的优势并不明显,可能需要大样本的随机对照研究才能得出结论。笔者认为:术者首先应选用最熟悉的固定方式做到坚强固定即可,同时还要考虑骨折的类型进行选择。
鹰嘴截骨端的固定方式:过去对鹰嘴截骨端均采用张力带固定,但有一部分患者出现骨折端分离、移位,延迟愈合或不愈合。目前许多医师喜欢采用钢板固定,认为固定坚强,但若肘周围软组织条件不佳,则可发生切口裂开及钢板外露,必须综合考虑钢板固定的优势和风险。因为鹰嘴截骨为简单骨折,建议采用张力带固定,内固定物越少,后期功能恢复越佳,软组织出现问题的可能也越小,术后功能锻炼要避免强力被动牵拉训练,否则可发生创伤性骨化,造成肘部僵硬。而对于截骨端不稳定或骨质疏松患者可考虑采用钢板固定,必要时可两者相结合。
尺神经是否前移:肱骨髁间骨折后路手术时,必须显露并全程保护内侧的尺神经,在手术结束时将其在无张力下与内固定物相间隔,但是否需要前移仍存争议,笔者通常进行以筋膜束将尺神经前置于屈肌腱浅层,以避免屈肘时张力过大以及与钢板的接触粘连。
全肘关节置换
全肘关节置换(TEA)最早用于治疗肘关节类风湿性关节炎、骨性关节炎和创伤后关节炎。但近10年来,已广泛应用于低位粉碎、关节面严重破坏、严重骨质疏松的老年患者。TEA治疗髁间骨折的适应证为年龄>65岁(老年人标准,发达国家为≥65岁,发展中国家为>60岁)、剧烈活动少、骨质疏松明显、骨折粉碎难以良好复位和有效固定,可较好地恢复患者的肘关节功能,提高老年人生活质量。对伴有炎性关节病,如类风湿、银屑病,关节已遭不同程度破坏的骨折患者,TEA的疗效更佳。但笔者建议严格把握年龄和手术适应证,对可获得牢固固定、开放骨折和体力活动较多者,禁忌行TEA。任何假体置换都有其固有的问题及并发症,对较年轻的肱骨髁间骨折还是应首选切开复位内固定。
肘关节复杂骨折脱位
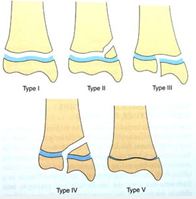
肘关节复杂骨折脱位可分为三大类(5种类型),即后外侧旋转不稳定(包括MasonIV型桡骨头骨折和肘关节三联征)、经鹰嘴骨折脱位(向前或向后两种)、内翻-后内侧旋转不稳定。
后外侧旋转不稳定(PLRI):通常是摔倒时手部撑地,肘部受到外翻、旋后和轴向应力,尺骨近端相对滑车发生向后外侧移位。接着发生一系列损伤,自外侧开始,向前或向后旋转至内侧,此种损伤类型通常称为Horii环。外侧副韧带(LCL)复合体常自其外上髁止点撕脱,是最早损伤的结构之一。内侧副韧带前束则是最后的受损结构,肘关节脱位时内侧副韧带前束也可能保持完整。根据能量消散的方式不同,这种损伤可造成单纯关节囊韧带损伤和单纯肘脱位,也可造成复杂骨折脱位,即肘脱位伴桡骨头骨折(即MasonIV型)或肘脱位伴桡骨头和冠状突骨折(即肘关节三联征)。后者因易引起陈旧性持续不稳定和创伤后关节退变,治疗效果不佳,被称为“恐怖”或“可怕”三联征(terribletriad),但随着手术技术和治疗理念的进步,也可获得满意疗效,因此建议将其统称为“肘关节三联征”。此类损伤的治疗目标是:重建肘部同心圆性复位及可靠的稳定性;术后早期活动,恢复良好的功能;减少并发症。
治疗原则及流程:(1)急诊尽量先行手法复位并临时制动;(2)通常可通过单一的外侧入路按由深至浅的顺序进行固定,即先固定冠状突,再固定或置换桡骨头,最后修复LCL,只有少数情况下若显露或操作困难可考虑加用内侧入路;(3)重建冠状突稳定性,尽量复位内固定,若骨折块太小或粉碎不能行内固定,则套索缝合前方关节囊;(4)重建桡骨头稳定性,尽量复位内固定,不能固定者则可考虑金属假体置换;(5)修复LCL复合体、伸肌总腱止点和(或)后外侧关节囊,可采用经骨缝合或用缝合锚修复;(6)经上述操作后,肘部仍不能达到同心圆性中心复位或稳定性仍不能达到早期活动的要求,则使用可活动的铰链外固定架;(7)术后注意早期功能康复治疗。
经鹰嘴骨折脱位:经鹰嘴骨折脱位包括半月切迹断裂、桡骨头骨折和(或)脱位、冠状突骨折,即肘部所有骨性稳定结构均发生损伤,可分为向前和向后两类。向前或经鹰嘴骨折脱位:经鹰嘴的肘关节骨折脱位常因在屈肘时前臂背侧受到高能量直接打击所致。此类损伤表现为尺骨鹰嘴或尺骨近端复杂骨折,前臂向前脱位,上尺桡关系正常,尺骨近端结构获得解剖复位固定后,肘部常可恢复稳定。
向后骨折脱位或向后孟氏损伤:向后孟氏损伤是肘关节向后骨折脱位的其中一种类型。常由摔倒时肘关节着地所致,表现为桡骨头向后脱位,尺骨近端粉碎骨折,冠状突骨折(基底部骨折第2亚型),肱尺关节不稳定。与向前的经鹰嘴骨折脱位相反,恢复骨性稳定结构后,肘关节可能仍然存在不稳定。
这两类损伤均可采用后正中切口,经骨折端对冠状突和半月切迹进行复位和固定,并用钢板对尺骨近端进行坚强固定,接着采取Boyd入路或外侧Kocher入路对桡骨头进行固定或置换。安装假体时要避免发生“过度填塞”,即假体位置不能过高,否则不仅影响肘屈伸,也可导致前臂旋转障碍。通常恢复骨性结构后可获得良好的稳定性,个别患者需要修复LCL。
内翻-后内侧旋转不稳定(V-PMRI):内翻-后内侧旋转不稳定常因摔倒时肩关节外展前伸、上肢伸直、手部撑地,使前臂受到内翻、后内侧旋转及轴向应力,造成LCL复合体自外上髁止点撕脱,同时冠状突内侧缘撞击内侧滑车,导致冠状突前内侧面骨折。此种不稳定可仅表现为轻度的关节不匹配,易漏诊,很快造成关节退变。应避免漏诊,积极手术治疗,对冠状突骨折采取内侧支撑钢板结合克氏针进行固定,修复LCL或用铰链式外固定架固定。
肘关节僵硬松解
当肘关节活动不能达到功能活动范围时,可定义为肘僵硬,而功能范围的定义不断改变。1981年Morrey等提出日常生活中肘功能活动范围是屈伸100°(即伸肘受限30°至屈肘130°),前臂旋转100°(即旋前50°/旋后50°),只要保留这200°的活动范围即可满足绝大多数日常生活及工作需要。但2011年Sardelli等重新定义了现代日常生活中的功能范围,认为现代日常生活所必须的肘关节功能活动范围比过去报道的范围更大。对创伤后肘僵硬严重影响上肢功能,保守治疗至少6个月仍无效,有强烈改善功能愿望者,可考虑采取手术松解,其疗效可靠。而一部分特殊职业者,即使其肘活动可达到比较满意的功能范围而仅有轻度的伸肘或屈肘受限,也会要求改善关节活动,目前也逐渐将此类患者纳入关节松解的范围,可行切开或关节镜下松解。对关节面破坏、缺乏透明软骨覆盖者,不能单纯行关节松解术,而应采取间隔式关节成形术。对老年患者,可进行人工全肘置换。而存在活动性感染、皮肤条件差、患者依从性差则为手术禁忌。
严重肘僵硬的患者常合并有不同程度的异位骨化十分常见,其手术时机仍有争论。一般认为应在异位骨化成熟后切除,目前大多建议在伤后6个月切除,若异位骨化切除过早,容易导致其复发;若切除过晚,由于肘部周围组织挛缩加重,关节软骨退化明显,则可使切除后的疗效不佳。Garland等提出,若异位骨化合并脊髓损伤者,则建议在伤后1年切除;合并脑部损伤者,建议在伤后18个月切除。笔者认为对于这类患者也可尝试保守治疗6个月仍无效即可尽早手术,避免关节软骨退变。术前可给予单次局部低剂量放疗或术后口服非甾体类抗炎药物预防异位骨化复发。
选择手术入路应考虑既往存在的手术切口,异位骨化的部位、范围及有无尺神经症状,是否存在前臂旋转受限等。为最大限度恢复活动范围,术中应进行彻底松解,目前常用的是后正中切口或内外侧联合切口。
采取内外侧联合入路可清楚显露前、后方关节囊及增生组织,并可完整切除之,也可对尺神经进行松解。若患者已存在后侧切口,也可以再次采用,其优点是可完整显露内、外侧,缺点是需要广泛剥离,术后锻炼时切口所受张力较大,可出现皮下血肿、皮肤坏死等。笔者曾对肘松解时采用的后正中入路和内外侧联合入路进行了对比研究,发现两种手术入路均可进行有效的松解,获得明显的功能改善,但内外侧联合入路可避免后正中入路时的切口并发症,如血肿、切口裂开等。
对严重肘僵硬者,术中需要彻底松解,即使对松解的LCL(特别是LUCL)进行重新附丽,也可能造成术后关节不稳定,或术者因忌惮术后出现不稳定而没有彻底松解。对此类患者,可在彻底松解后加用可活动的铰链式外固定架,有助于最大限度恢复关节功能并维持关节稳定,还可用外固定架牵开关节间隙。笔者曾通过对照研究,发现用铰链式外固定架者尽管术前僵硬程度更重,但术后活动范围改善明显优于不用外固定架的单纯松解者。
肘关节创伤的病种繁多,要提高我国的肘关节治疗水平,最重要的是要具有先进的治疗理念,掌握基本的治疗原则和治疗方法,通过早期合理的治疗,提高治疗效果,改善患者功能,而不是盲目追求最新的固定方式或内固定物。早期恢复肘部正常的骨性和软组织解剖结构非常重要,即使功能活动范围不佳,也可通过II期松解手术改善关节功能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肘关节#
33
不错哦,会学到很多,喜欢梅斯医学文章
66
好文,值得学习,赞!
79
骨科这种都是经验出真理啊
112
#损伤#
20
去学习吧
93
有用有用
73