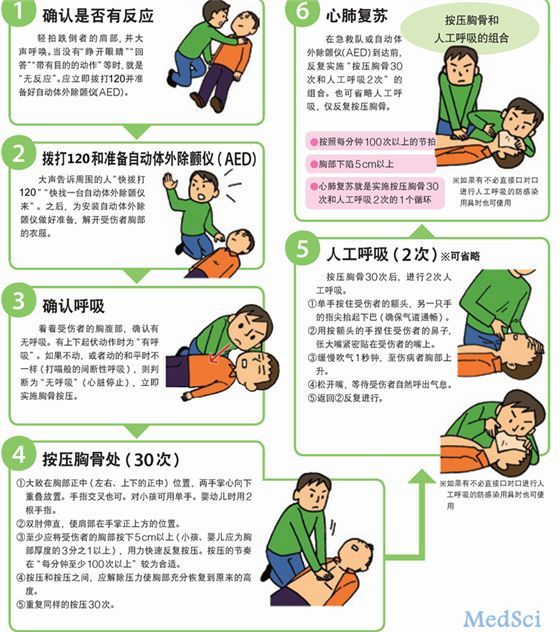
《2016中国心肺复苏专家共识》出台,普通人仅需知道五步
2017-02-13 杨进刚 中国循环杂志
近日,指导我国心脏停搏综合防治体系构建和心肺复苏(CPR)临床实践的行动指南——《2016中国心肺复苏专家共识》(以下简称《共识》)正式出炉。该《共识》由中国研究型医院学会心肺复苏学专业委员会汇集国内CPR领域专家,基于国际CPR指南的科学共识,结合我国国情和具体实践,涵盖了心脏停搏前期的“预防、预识、预警”的“三预”方针、心脏停搏中期的“标准化、多元化、个体化”的“三化”方法与心脏停搏后期“复生
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













对于普及CPR很有用
74
#专家共识#
29
学习了,谢谢。
56
#心肺#
31
非常的有用
72
#复苏#
24