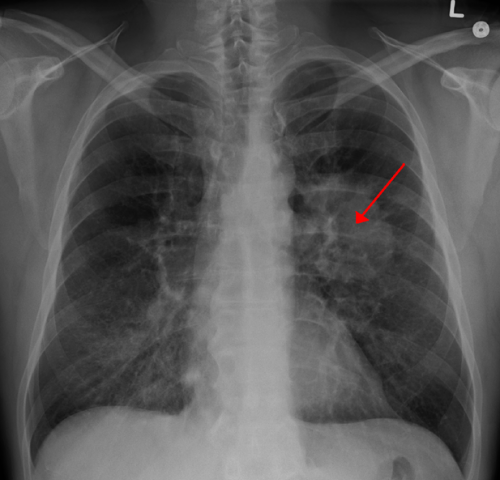
得了这种病,吹肥皂泡都成了一种奢望!不是癌症的癌症,识别危险信号,早诊早治!
2018-01-10 佚名 健康时报
不能爬楼梯,一爬就气喘;不能干家务,一动就气喘,咳嗽;连吹肥皂泡也成了一种奢望。他们的肺仿佛被一张无形的网勒紧,束缚着他们的日常行动和生活。对于常人来说再自然不过的“呼吸”,却成为他们四处奔走、渴望达成的目标。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#危险信号#
34
谢谢了.学习
75
好
77
#早诊早治#
35
受益
75
学习了很有用
70