JAMA:司美替尼(selumetinib)对葡萄膜黑色素瘤的治疗优于化疗
2014-06-23 MedSci MedSci原创
近日一项临床研究证实:一个疗法已被发现,可延缓转移性葡萄膜黑色素瘤进展,葡萄膜黑色素瘤是一种罕见的致命形式的眼黑色素瘤。 几年前,研究人员发现80%的葡萄膜黑色素瘤患者有GNAQ或GNA11突变,GNAQ和GNA11基因激活MAPK信号通路。Schwartz博士等人后来证明,抑制MEK(在MAPK途径中的关键酶)可以抑制实验室中葡萄膜黑色素瘤细胞生长。在2013年,Schwartz博士和
近日一项临床研究证实:一个疗法已被发现,可延缓转移性葡萄膜黑色素瘤进展,葡萄膜黑色素瘤是一种罕见的致命形式的眼黑色素瘤。
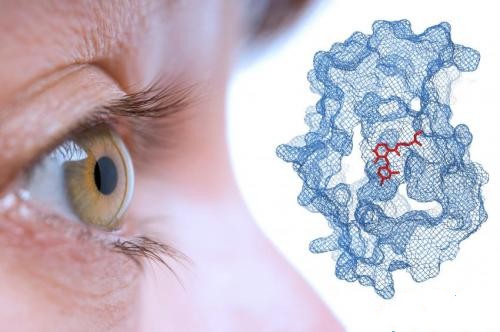
几年前,研究人员发现80%的葡萄膜黑色素瘤患者有GNAQ或GNA11突变,GNAQ和GNA11基因激活MAPK信号通路。Schwartz博士等人后来证明,抑制MEK(在MAPK途径中的关键酶)可以抑制实验室中葡萄膜黑色素瘤细胞生长。
在2013年,Schwartz博士和他的同事们发起了第一次大规模,selumetinib的二期随机试验。其中美国和加拿大的15个中心101 例转移性葡萄膜黑色素瘤被随机分配接受selumetinib或标准化疗。如果这些化疗组的患者表现出疾病进展的迹象,可以随时再接收 selumetinib治疗。该研究结果发表在近日的JAMA杂志上。
接受selumetinib患者中位无进展生存期比接受化疗患者的中位无进展生存期超过一倍(15.9周vs 7周)(HR=0.46; 95% CI, 0.30-0.71; P < .001)。49%的selumetinib治疗患者表现出肿瘤消退。Selumetinib治疗患者中位总生存期为11.8个月,化疗组患者为9.1 个月(HR=0.66; 95% CI, 0.41-1.06; P = .09)。两组之间差异无统计学意义。Schwartz博士说:我们怀疑,selumetinib组患者生存有可能确实得到改善,但目前还不十分清楚,因为那些化疗耐受的患者被允许再接受selumetinib治疗。
绝大多数服用selumetinib患者经历的副作用包括皮疹,浮肿以及视力改变。大多数的副作用被认为是可管理的。Schwartz博士认为,治疗葡萄膜黑色素瘤,最终涉及到合理的药物设计和药物结合。在临床前研究中,研究已经证明当MEK抑制剂结合Akt抑制剂,结果比单独使用MEK时要好。Gary K. Schwartz作者说:虽然这种药物的作用是温和的,但现在我们知道,我们可以影响疾病进程。本研究的注册号:NCT01143402
MedSci专家也认为,对于这种较为罕见,且恶性度很高的葡萄膜黑色素瘤的来说,selumetinib不仅给患者提供多一种选择,而且就目前的数据而言,患者得到良好的获益。虽然,这项研究尚未观察到患者对OS的获益,可能与次要终点的设置有关。从这个数据上看,患者得到2.7个月的获益,这已经是相当不错的进步,下一步有必要针对OS再开展单独的临床试验,证实selumetinib对葡萄膜黑色素瘤的OS获益可能。同时,还要开展selumetinib作为二线治疗带来的获益,以及selumetinib作为一线治疗后再用化疗,还是先用化疗再用selumetinib作为二线治疗进行对比,了解哪些方案更加优化。甚至将来还应该进行更深入地研究,由于selumetinib毒副作用相对较小,因此,可以考虑两种靶向药物的联合治疗,可能会使患者能得到更深层次的获益,期待这些研究的问世。
原始出处:
Carvajal RD, Sosman JA, Quevedo JF, Milhem MM, Joshua AM, Kudchadkar RR, Linette GP, Gajewski TF, Lutzky J, Lawson DH, Lao CD, Flynn PJ, Albertini MR, Sato T, Lewis K, Doyle A, Ancell K, Panageas KS, Bluth M, Hedvat C, Erinjeri J, Ambrosini G, Marr B, Abramson DH, Dickson MA, Wolchok JD, Chapman PB, Schwartz GK.Effect of selumetinib vs chemotherapy on progression-free survival in uveal melanoma: a randomized clinical trial.JAMA. 2014 Jun 18;311(23):2397-405
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#色素#
23
#MET#
27
#葡萄膜黑色素瘤#
33
#黑色素#
27
#黑色素#
26
#司美替尼#
25