OCC 2020:聚焦多模态影像技术,寻找稳定性冠心病诊疗新策略
2020-06-02 MedSci原创 MedSci原创
5月28日,第十四届东方心脏病学会议(OCC)于云上东方线上平台召开,多位临床专家汇聚一堂,为大家带来心脏病学领域的饕餮盛宴。
5月28日,第十四届东方心脏病学会议(OCC)于云上东方线上平台召开,多位临床专家汇聚一堂,为大家带来心脏病学领域的饕餮盛宴。
冠心病介入论坛版块的多模态影像技术指导冠心病精准治疗论坛涵盖了多模态影像技术、放射性核素心肌血流定量新技术、高分辨专业型CT、心脏超声在心血管诊疗中的临床应用价值、CQK心脏科研平台及FFR技术等多样化研究。

图片来源:OCC会议官网
来自解放军总医院心血管病医学部的陈韵岱教授向我们分享了多模态影像技术指导冠心病精准治疗的精彩内容,介绍了《稳定性冠心病无创影像检查路径的专家共识》[1],该专家共识于2017年10月发表于陈韵岱教授主编的《中国介入心脏病学杂志》,此共识帮助我们重新审视稳定性冠心病诊疗流程方面的困惑。
图片1.《稳定性冠心病无创影像检查路径的专家共识》
《稳定性冠心病无创影像检查路径的专家共识》内容介绍
针对共识中引入的验前概率(PTP)的概念,陈教授做了详细阐述。冠心病 PTP是根据临床综合情况, 初步推测患稳定性冠心病的可能性, 是合理选择无创影像技术的关键环节[1]。疑似冠心病患者在正式确诊之前,需要进行一系列无创或有创功能学检测,同时心血管临床医师需要考虑这部分患者阳性率和阴性率问题。共识中同时包含明确的运动负荷和药物负荷对缺血的判定,如果患者未出现高危缺血则进行常规药物治疗,反之则进行相关介入治疗。
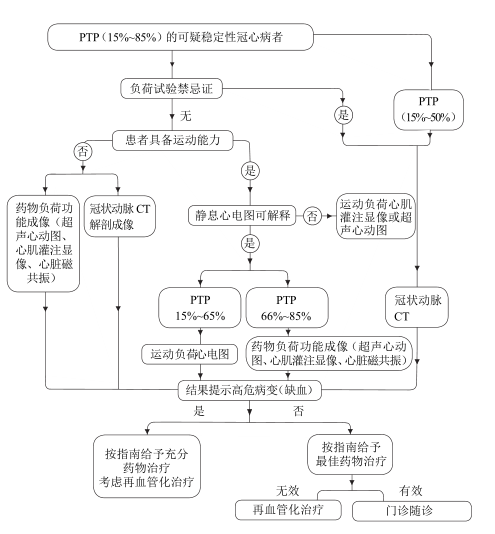
图片2.可疑稳定冠心病且验前概率 (PTP) 为中等 (15%~85%)的患者无创影像检查路径
疑似冠心病患者一经确诊,是否只需在导管室观察病变血管狭窄程度呢?
显然不是!陈教授对该问题的解答是:确诊冠心病的患者,心血管临床医师仍需通过个人运动能力评估患者缺血范围,从而判定患者有无严重缺血。
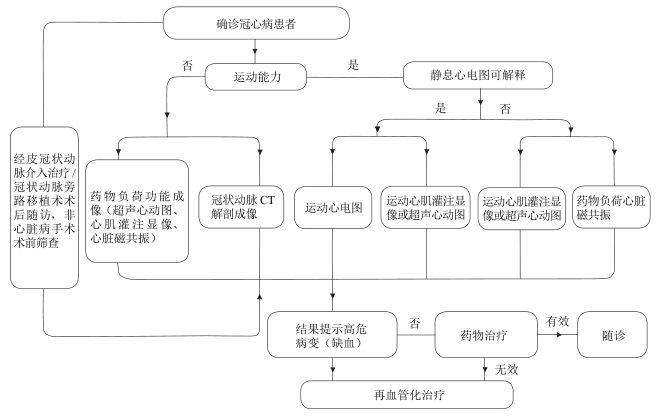
图3.确诊冠心病的患者评价心肌缺血状态的无创影像检查路径
共识中提及的平板运动(最常用的运动心电图负荷试验检查方式)为什么不易被患者接受?
陈教授:平板运动试验不能直接反应冠状动脉病变情况,但是具有经济、简便、实用、相对安全、无创性和可重复性的优点。在临床上,优先推荐无创影像检查技术,可参考《稳定性冠心病无创影像检查路径的专家共识》对患者进行分层。对于稳定性冠心病患者,无创影像技术的不仅能判断斑块的狭窄程度,还能评估患者的缺血范围和高危性。

图4.无创影像检查技术在临床优先推荐
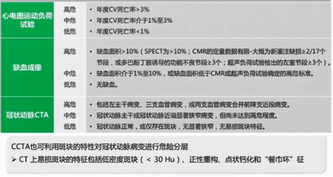
图5.无创影像检查对稳定性冠心病患者的危险分层
陈教授以CT技术为例分享多模态影像技术指导冠心病诊疗进展
目前,冠心病救治方面的困惑已从结构向功能学转变,因此与疾病症状相对应的功能学成为心血管临床医师关注的焦点。CT“一站式”检查已日益在临床得到应用,该检查既评估斑块狭窄程度,又通过CT血流动力学(FFRct)和CTP动态定量分析进行疾病缺血范围的界定。
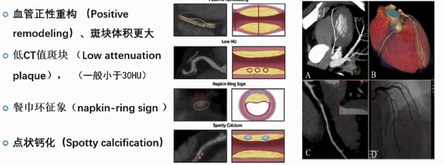
图6.CT易损斑块的识别
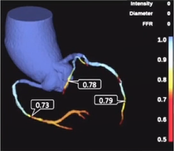
图7.CT血流动力学(FFRct)

图8.CTP动态定量评价
未出现明显斑块狭窄和严重缺血的冠心病患者可以避免介入治疗正是得益于CCTA/FFRct“一站式”策略。
陈教授带领的团队在2017年SCCT(国际心血管CT学会年会)会议上发布动态灌注心肌成像方法学的研究成果,利用该技术建立了“一站式”心脏CT功能学评价方法学,不仅实现了冠状动脉形态学的评估和心外膜冠状动脉狭窄的功能学评价,还可同时实现心肌水平灌注的评估。
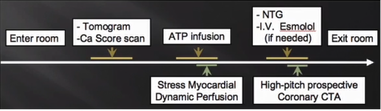
图片9.动态心肌灌注成像的方法学
分享两个典型病例
患者1:男性42岁,典型心绞痛
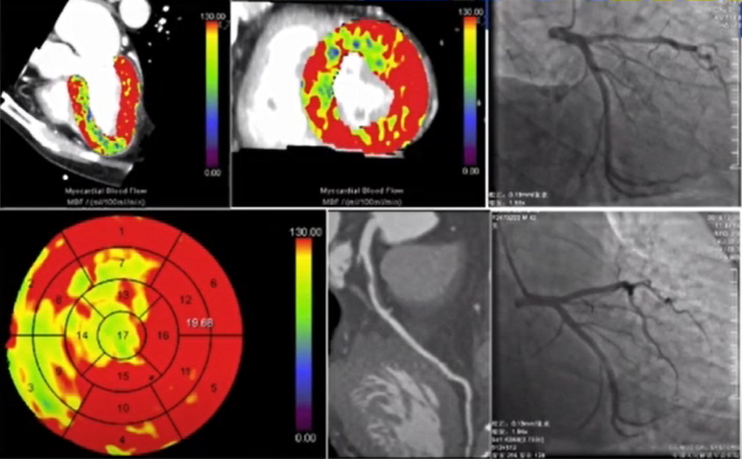
图片10.冠脉CTA提示前降支近端重度狭窄合并明显的心肌灌注缺损区域,随后的冠脉造影证实局限性重度狭窄,最终在冠脉病变区域植入DES支架一枚
患者2:女性66岁,不稳定性心绞痛
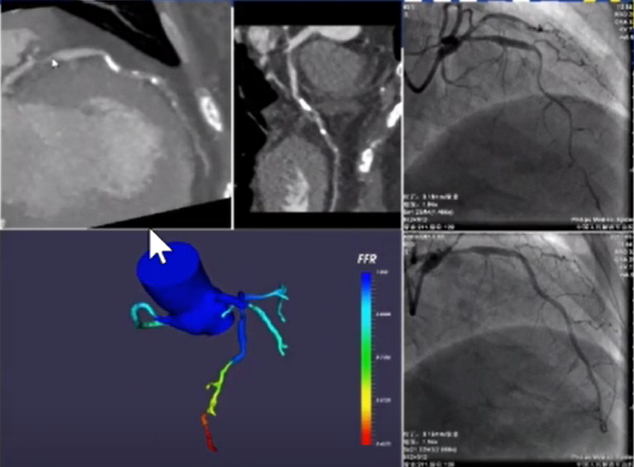
图片11.冠脉CTA提示前降支弥漫长病变,国产化FFRct提示近端病变压力变化不明显,远段FFR值为0.57,随后的冠脉造影及FFR证实远段压力值明显降低,开通中远段血管后FFR明显改善,前降支近端病变对应的FFR值为0.87,故未进行介入干预
解放军总医院陈韵岱、杨俊杰团队发表于JACC : C ARDIOVASCULAR IMAGING中的一项研究中发现了从动态CTP中衍生出的一个新参数SFR,它可以准确地估计有创性FFR,从而识别有血流动力学意义的冠状动脉狭窄。相比MBF,SFR在判断有血流动力学意义的狭窄病变中有更高的特异性、阳性预测价值及诊断准确性(分别为91%,85%和80%),而敏感性及阴性预测价值有限(分别为62%和73%)[2]。

图片12. Yang Junjie,Dou Guanhua,He Bai et al. Stress Myocardial Blood Flow Ratio by Dynamic CT Perfusion Identifies Hemodynamically Significant CAD.[J] .JACC Cardiovasc Imaging, 2020, 13: 966-976.
引用最新重磅研究,进一步阐述多模态影像技术在冠心病诊疗方面的临床应用价值
最后,陈教授强调冠脉CTA应作为冠心病诊断的一线方案,并引用2018年发表于The New England Journal of Medicine的SCOT-HEART研究[3],该研究结果显示:疑似冠心病患者CTA检查可显著降低硬终点风险达38%。
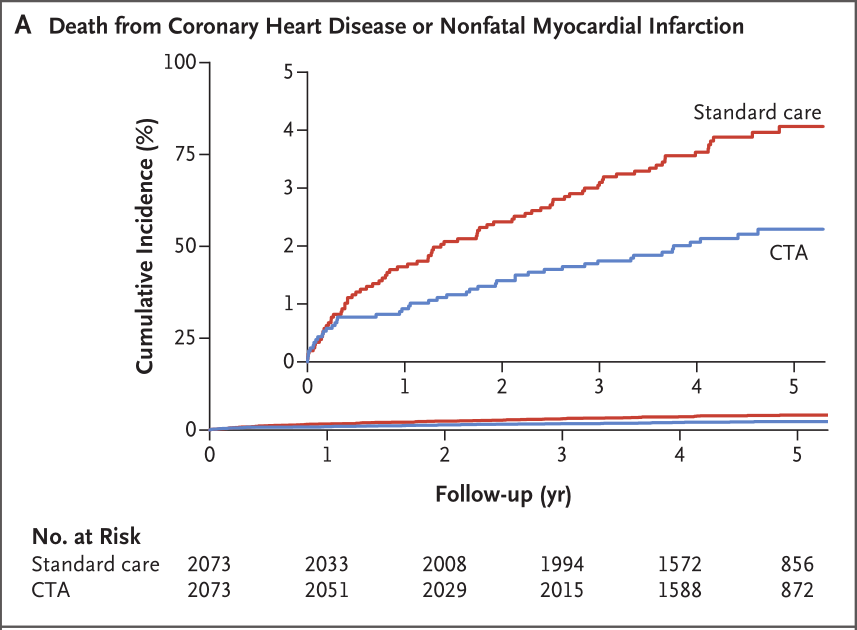
图片13. 死于冠心病或非致命性心肌梗死
另外,发表在The New England Journal of Medicine的核磁心肌灌注指导介入治疗MR-INFORM研究[4]亦不容小觑,该研究结果显示:MRI指导治疗效果不劣于FFR。
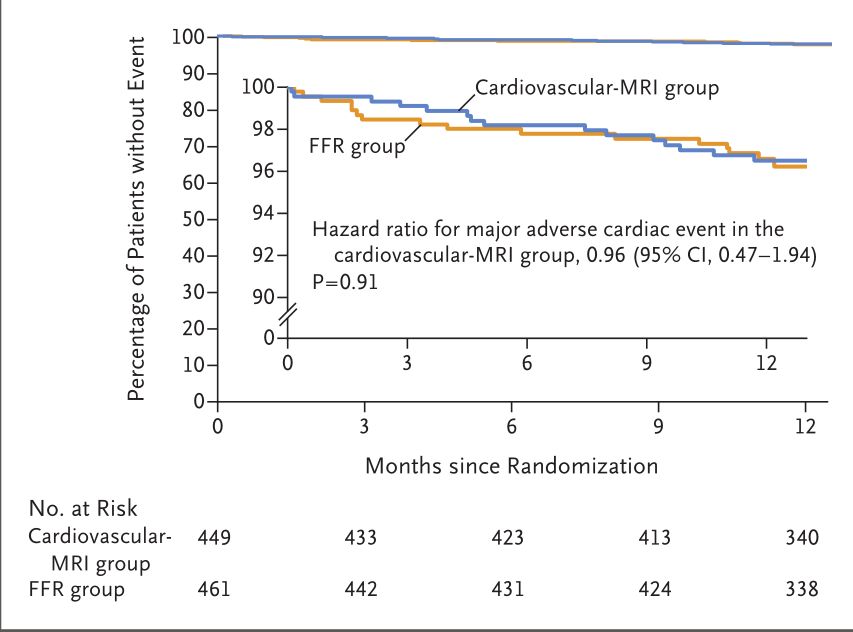
图片14. Kaplan–Meier对不受主要综合结果影响而存活的患者的分析
2019AHA重磅结果,ISCHEMIA研究结果[5]显示:不能使稳定性冠心病患者更多获益,关键硬终点均未见显著差异。这就需要心血管临床医师在针对稳定性冠心病患者的评估过程中灵活应用新方案。
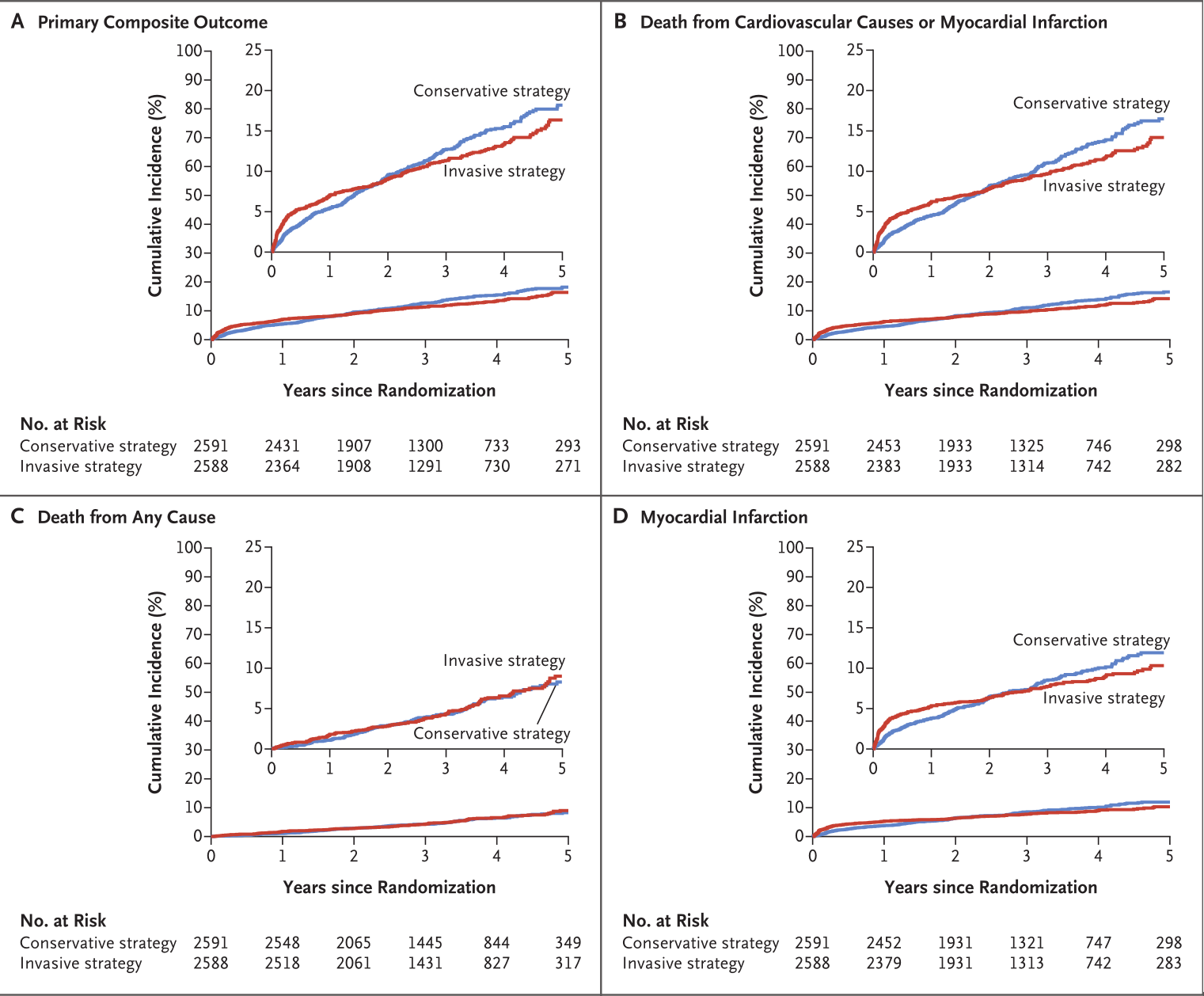
图片15. 主要综合结果和其他结果的事件间隔时间曲线
因此,只有充分了解各项无创影像检查技术,才能在临床应用中进行合理选择,既不过度医疗又可有效检出冠心病患者。如果我们充分发挥多模态影像技术的联合优势,能更好地为临床工作服务。
参考文献:
[1] 稳定性冠心病无创影像检查路径的专家共识[J].中国介入心脏病学杂志,2017,25(10):541-549.
[2] Yang Junjie,Dou Guanhua,He Bai et al. Stress Myocardial Blood Flow Ratio by Dynamic CT Perfusion Identifies Hemodynamically Significant CAD.[J] .JACC Cardiovasc Imaging, 2020, 13: 966-976.
[3] SCOT-HEART Investigators,Newby David E,Adamson Philip D et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction.[J] .N. Engl. J. Med., 2018, 379: 924-933.
[4] Nagel Eike,Greenwood John P,McCann Gerry P et al. Magnetic Resonance Perfusion or Fractional Flow Reserve in Coronary Disease.[J] .N. Engl. J. Med., 2019, 380: 2418-2428.
[5] Maron David J,Hochman Judith S,Reynolds Harmony R et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease.[J] .N. Engl. J. Med., 2020, 382: 1395-1407.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#稳定性冠心病#
79
#稳定性#
36
#多模态#
33
#OCC#
27
#OCC 2020#
39
#新策略#
35