ISRD & ATS 2016:张国桢教授谈微小肺癌影像诊断与鉴别要点
2016-10-18 MedSci MedSci原创
2016 年10月14日~16日,由上海梅斯医学承办的“第十二届上海国际呼吸学会暨ATS联合论坛”(ISRD & ATS 2016)在上海展览中心隆重举行。14日下午,复旦大学附属华东医院张国桢教授作了题为“微小肺癌影像诊断与鉴别要点”精彩演讲。梅斯小编对张国桢教授的精彩报告进行整理,与大家分享。复旦大学附属华东医院张国桢张国桢教授介绍说,21世纪是一个从经验医学走向循症医学——精准医学c
2016 年10月14日~16日,由上海梅斯医学承办的“第十二届上海国际呼吸学会暨ATS联合论坛”(ISRD & ATS 2016)在上海展览中心隆重举行。14日下午,复旦大学附属华东医院张国桢教授作了题为“微小肺癌影像诊断与鉴别要点”精彩演讲。梅斯小编对张国桢教授的精彩报告进行整理,与大家分享。

张国桢教授介绍说,21世纪是一个从经验医学走向循症医学——精准医学combine的时代。是应用现代化的医学技术,明确地将现有的可靠证据,精准的地应用于诊断决策中,然后对病人的权益、价值、期望三结合以制定出个性化的预防与治疗方案。其中精准医学包括4个要素:精准诊治(the right diagnosis&treatment)、精准时间(at the right time)、互相共享(give all of us access)、重个体化(personalized information)。
张国桢教授从以下六个方面进行了阐述:
一、肺微小结节影像学的处置原则:
低剂量CT肺癌筛查≠照相馆
低剂量CT 筛查可得到0.06mSv=3张胸片的X线剂量,Ⅰa期肺癌的发现率从35.1%提高至93.0%。但也可发现更多肺内微小结节,通常是数量较多、大小不一、新旧交替、种类复杂、多无特征、良恶不明。这就给诊断带来新的问题。因此,提高早期肺微小腺癌的诊断和鉴别诊断水平始终是影像学研究的重要课题。
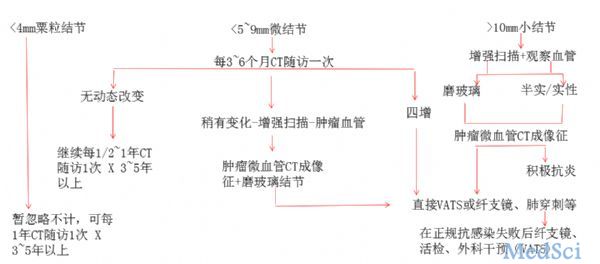
张国桢教授还说,偶然发现的肺结节有三种:实性结节(Solid Nodule)、部分实性结节(Part-solie Nodule)和磨玻璃结节(Ground-glass Nodule)。对于实性结节和部分实性结节来说,影像处置原则如下:
粟粒结节(≤4mm),暂可忽略不计;微结节(5-9mm),抗炎治疗2个月后复查CT;小结节(≥10-20mm),抗炎治疗2个月后复查CT+增强扫描。
张国桢教授说,力争将肺癌扼杀在0期,把握好AIS的影像诊断是关键。根据第七版UICC TNM病理分期标准,肺癌五年生存率如下表,而0期(原位癌Tis)的5-10年生存率是100%。

在0期微小肺癌的CT影像诊断中,传统的肺癌影像诊断标准(如分叶、毛刺、胸膜凹陷等)已经不适用。根据亚厘米微小肺癌的肿瘤生物学发展行为,现提出新的综合性诊断技术方案:
2、CT技术具有新模式;
3、处置原则具有新理念。
二、0~ⅠA1期微小肺癌影像诊断的新标准
发现1:“肿瘤血管”,肿瘤微血管CT成像征或称肿瘤微血管移动-联通征。
发现2:微小肺癌的血供具有随机性,可以是肺动脉,肺静脉,支气管动脉来源。
发现3:(与传统观点不同)增强CT扫描对于判断微小肺癌的影像诊断非常重要。
三、肺微小结节三维图像后处理技术是发现肿瘤微血管的基石
CT横断面图像的传统模式已不能满足临床要求,寻找GGN的肿瘤微血管CT成像征应采用CT技术图像后处理的新模式:最大密度投影(maximun intensity projection,MIP)、多平面图像重组(multi-planar reformation,MPR)、曲面重组(curved planar reformat,CPR)、容积再现(volume rendering technique,VRT)二维、三维图像后处理。这已成为发型肿瘤血管的基石,极大地提高了对微小肺癌,特别是AIS与MIA影像诊断的精准性。
另外,张国桢教授还介绍了离体肺标本充气下CT导向穿刺定位微小结节的创新方法。
四、0~ⅠA1期微小肺癌诊断处置原则的新理念:诊治端口要前移,重点必须在零期。
张教授还提到“四抓”和“四增”。
“四抓”是抓早(0期Tis)、抓小(亚厘米肺癌)、抓准(术前正确定性定位)、抓好(胸外、放射、病理科协作,提高5mm小病灶病理取材准确性)。“四增”是指增大、增密、增强、增粗(肿瘤血管)。
结节内的实变与生长速度的加快提示为恶性征象,在GGN随访期间,一旦出现病灶增大、有实性出现增密、结节有增强、有移动血管增粗这“四增”时,应停止随访,建议做手术(VATS),以免延误早期肺癌的诊治。所以极需要把握好“四抓”“四增”新原则以及AIS的影像及病理诊断,提高0期肺腺癌的检出率,及早启动干预,保证患者的生活质量和寿命,将肺癌诊断和治疗的关口前移才是提高肺癌治疗水平与提高肺癌五年生存率的关键所在。
张教授举例说,磨玻璃灶中密度增加的实变部分,在病理上是肿瘤的浸润性生长部分。每当CT值增加100HU时,也就意味着肿瘤的体积增加10%。
五、微小肺癌CT形态新的10种分型及演变转化规律
对肺癌病灶的影像分析要点可概括为“五定”,即定位、定量、定性、定性、定级。其中定位置、定数量、定级别(TNM分期)都必须是在对肺分叶、分段及纵隔淋巴结分组解剖结构熟知的基础上才能判断无误。定形、定性则是依靠肿瘤的形态学、功能学的特征来完成的。
在肺腺癌发生、发展过程中的早期阶段,其发生的部位可以是在肥泡、肺泡管,也可以是在呼吸性细支气管、肺小叶支气管等各种不同部位,这就可以造成肿瘤各不相同的影像形态。又由于肿瘤在不同区域的发展往往是不同步的,在同一肿瘤的某些区域可以表现出停滞不前的状态,在另外区域则表现出退缩状态,又有些区域还可表现出很活跃的状态,这同样也可以造成肿瘤有各不相同的影响形态。这两个病理基础就造成肺腺癌在CT影像上可以呈现10种类型的形态改变,从而才能对微小结节肺癌作出精准的CT诊断。
在解剖学上肺泡管是人体肺呼吸系统的重要组成结构,它是指从肺泡囊到呼吸性细支气管的通道,也由肺泡围成。有小团状的平滑肌断面和单层扁平上皮,因此当肿瘤沿肺泡管长轴方向浸润伸展,黏膜呈隆起的结节状增生,管壁增厚,肿瘤局限于管腔内。CT表现为细小串珠状的磨玻璃病灶。肿瘤在细支气管壁内生长,表现为黏膜管壁的增厚。
根据其生长的长度和深度的不一,CT可以见到2种形态:
树枝型——细分支状,可以呈细条状(直径≤1mm)的磨玻璃密度影,见于连续数个相邻的层面上或在1个层面上相互紧挨排列。
另外,张国桢教授还介绍了瘢痕型肺癌。当一旦在原有的纤维硬结灶边缘出现软性的比较模糊的小点状及小片状灶或新出现胸膜皱缩、凹陷征时,这就提示是瘢痕癌早期的CT表现,此时尚未形成结节,这段最为困难,要特别引起注意。此种瘢痕往往位于瘤体中心,病理上常伴多量碳末沉着。
肺瘢痕腺癌的生长速度缓慢,倍增时间长,可达多年之久。因此对肺瘢痕癌诊断意义最大的仍是定期随访,观察CT影像上病变形态的变化甚为重要。在随访中病灶逐渐增大,在原有的纤维灶边缘周围出现较模糊的小点状及小条片灶或新出现胸膜皱缩、凹陷征时,纵隔淋巴结由小变大,则符合由肺纤维瘢痕灶发展到肺瘢痕癌的临床表现,具有肯定的手术指征。
六、肺微小结节影像学诊断原则与处理流程(总结)
1、据统计有15%的纯磨玻璃结节可以发展成恶性的,而且当直径>15mm后,其高危程度、恶性因素也随之增加。所以凡是正常人体检发现的长期存在的偶发性磨玻璃结节,经过抗炎或较长时期的观察不消失,且具有“肿瘤微血管CT成像征”时,要考虑肺原位癌的诊断。由于“肿瘤微血管CT成像征”的含义是:肿瘤血管移动进入瘤体+瘤体内微血管的互相联通,因此对于肺原位腺癌的CT诊断也可以简化为如下公式:
肺原位癌=体检发现的、长期存在的、偶发性纯磨玻璃结节+肿瘤微血管CT成像征
2、值得提醒的是千万不能以5mm的底线来划分结节的良恶性,因为实践证明4~5mm大小的AIS(原位腺癌)和MIA(微浸润癌minimally invasive adenocarcinoma,MIA)并不在少数。
3、通常约有50%的半实行结节是恶性的,而实性结节恶性的比例低于半实性结节,当然结节越大,其高危程度、恶性因素也随之增加。因此对于恶性概率较大的GGN,10mm以下的pGGN 6~12个月随访,mGGN 3~6个月随访,随访期间出现边缘分叶、毛刺、内部有空泡或实性成分、有胸膜受累征象等,建议VATS手术切除。
4、对于恶性概率较小的结节,带血管的、圆形的实性结节很可能是良性的,可先行抗炎治疗后2个月复查,或者不做任何治疗6个月后行CT复查。
5、对于难以定性的肺结节,可以推荐其进行随访观察,随访期间一旦病灶出现“四增”特点:增大、增密、增强、增粗(肿瘤血管)中的1~2项时,建议VATS手术切除。
总结如下图:
你是否还记得小学课本的这样一段话:西沙群岛的海里是一半是水,一半是鱼。每个人都一个梦想,我的梦想是到祖国最需要医生的地方去。
本次梅斯医学受邀为南海联合医疗支援队招募志愿者,举办“谁是中国最美医生”活动
点击此处即可参与,中国最美医生可能就是你!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ATS#
42
学海无涯苦作舟
73
重视微小肺癌的诊断
60
不断学习不断进步
66
重视微小肺癌的诊断
71
学海无涯苦作舟
69
不断学习不断进步
24
重视微小肺癌的诊断
22
学海无涯苦作舟
32
不断学习不断进步
31