Cell:解惑!肿瘤坏死因子拮抗剂治疗不明原因肠炎为何经常无效?
2019-09-04 BioArt BioArt
克罗恩病是一种不明原因的肠炎,属于消化道慢性炎症,最终可能导致消化系统损伤甚至是功能丧失。其致病因素多种多样,比如高脂高糖饮食,不规律且快节奏的现代生活方式,遗传因素等等,这些因素可以引起消化道免疫系统异常活化,导致肠炎。近年来,诸多工作力图阐明肠炎发生发展的分子机制,并寻找治愈缓解的方法。而这些工作,往往建立在经典的以“抗体标记蛋白质”的研究方法上。当然了,单细胞测序技术的运用,为这一领域 ,带
单细胞测序是目前生物学研究极为有效的手段之一。其工作流程可简单描述如下:
1、测序:对每个细胞进行测序,检测每一个细胞的基因表达情况。
2、分类:将表达谱类似的细胞分为一类,并根据其基因标签,鉴定鉴别细胞类型
3、亚类:深入分析每类细胞内部表达谱的区别,探索定义新的细胞亚型。
4、联系:进一步研究各细胞类型之间的联系与相互作用。
5、应用:结合实验材料自身特点,力图分析和解决生物学问题。
美国纽约西奈山伊坎医学院研究团队在Cell杂志发表文章Single-Cell Analysis of Crohn’s Disease Lesions Identifies a Pathogenic Cellular Module Associated with Resistance to Anti-TNF Therapy,通过单细胞测序的方法,从克罗恩病病人的回肠样本中鉴定出了八类细胞,定义了新的细胞亚群,此外,还从临床上解释了为什么肿瘤坏死因子(TNF)拮抗剂对某些克罗恩病没有很好的响应。
1、测序
作者采用十三位克罗恩病病人的回肠样本,分别分离样本中炎症和正常的肠道固有层细胞,这里蕴含着肠道中数目最多,种类最为丰富的免疫细胞。同时,也抽取同一病人的血液单核细胞作为细胞对照。样品采集完毕后,进行单细胞测序。并且,对同一样品进行高效质谱检测。单细胞测序针对基因水平,高效质谱针对蛋白质水平,从而可以对这批病人样本有更为深入和全面的了解。
2、分类
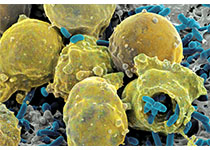
首先,作者从这些样本中主要鉴定出八类细胞,分别为树突状细胞(DC),巨噬细胞(Macrophage),固有层淋巴细胞(ILCs),肥大细胞(Mast cells),间质细胞(stromal cells),T细胞,单核吞噬细胞(mononuclear phagocytes),浆细胞(plasma cells)和B细胞。如下图所示,这些细胞,在炎症与正常组织中,含量存在明显的差异。
与此同时,比较炎症组织单细胞测序与高效质谱结果,可以看出,二者具有明显的相关性,也就是说,基因水平与蛋白质水平的变化是基本上一致的。
3、亚类
接下来,作者对这八类细胞进一步分析细化,力图定义新的细胞亚群。以树突状细胞为例,如下图所示,不同颜色代表某一基因不同的表达量,黄色表达量最高,紫色最低,黑色则是未表达。根据这些基因表达量的不同,可以把树突状细胞分成五个亚类。
4、联系
对比炎症组织与正常组织之间细胞含量的差异,可以看出IgG浆细胞(G),炎症性单核吞噬细胞(IM),活化的T细胞(AT)以及间质细胞(S)这四类细胞的比例明显增加,于是,作者将这四类细胞定义为一个细胞组,取其首字母定名为“GIMATS细胞组”。
为了进一步研究这一细胞组内部各细胞之间的关系,作者分析了各类细胞的表面受体和所分泌的细胞因子,并做一一比对。比如,巨噬细胞所分泌的一系列细胞因子,包括IL-1b,IL-6,IL-23,CCL2,CCL19,CCL22等,在T细胞表面都能找到相应的受体。
5、应用
最后,作者探究了这些结果的临床意义。
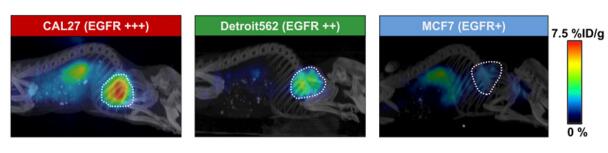
目前,肿瘤坏死因子(TNF)拮抗剂是治疗肠炎的药物之一。作者对接受这项治疗的病人进行分析,发现“GIMATS细胞组”含量高的病人,这一治疗方式的效果并不明显。也就是说,如果预先用这一方式对病人进行一次筛查,可以进一步提高TNF药物的治愈率。
这是一篇单细胞测序技术类文章的范本,严格遵循了“测序-分类-亚类-联系-应用”这一思路,定义了由IgG浆细胞(G),炎症性单核吞噬细胞(IM),活化的T细胞(AT)以及间质细胞(S)所组成的“GIMATS细胞组”,并且指出,这一细胞组是通过“细胞因子-表面受体”这一关系而紧密联系在一起,且与TNF治疗成败直接相关。该研究亮点主要有两处,一是采用人肠道组织为研究对象,这比用鼠等模式生物更具临床意义;二是不仅关注了一类细胞本身的变化,也重点关注了几类细胞的协同变化,这是单细胞测序技术结果分析的大势所趋。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
25
#Cell#
28
#坏死#
0
#肿瘤坏死因子#
38
#拮抗剂#
23