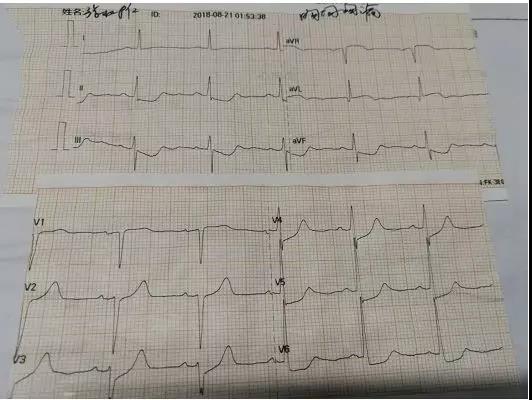
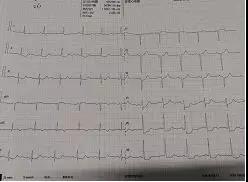
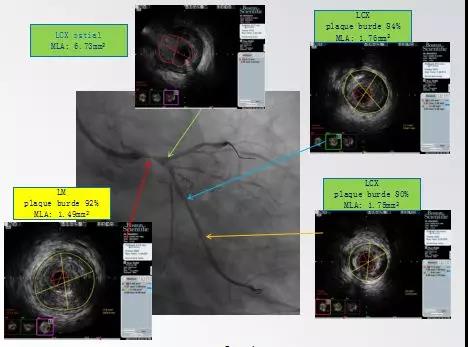
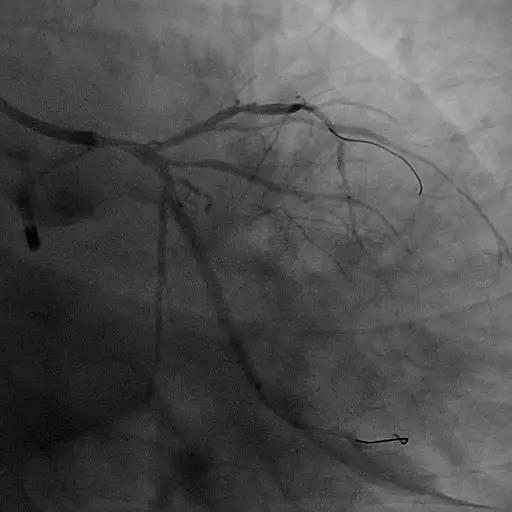
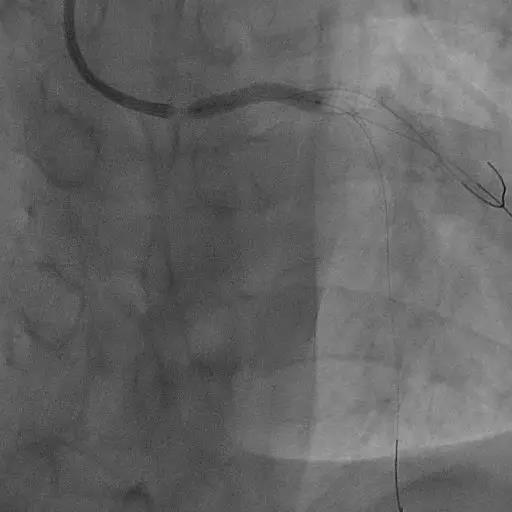
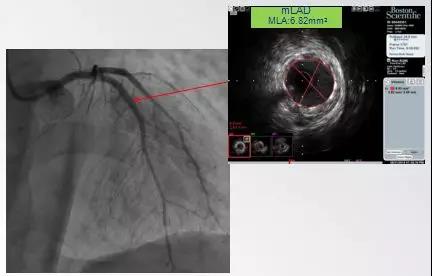
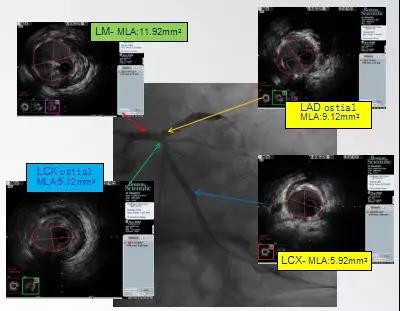
病例精选:IVUS指导下NSTEMI左主干闭塞病变优化PCI一例
2019-05-07 李辉 赵婕 王恒东 中国医学论坛报今日循环
张某,男,56岁因阵发性胸闷、胸痛4年,持续胸痛5小时急诊入院。





本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NST#
40
#左主干#
39
#STEM#
35
#NSTEMI#
39
#闭塞病变#
32