阑尾切除术-正常解剖、手术适应症、手术切口、手术过程和手术预后(图片)
2015-12-03 网络 MedSci原创
阑尾是细长的条索状肠组织,位于盲肠与回肠之间。 当发生急性阑尾炎时,必需施行紧急阑尾切除术,避免阑尾穿孔导致全腹感染(腹膜炎)。 急性阑尾炎的症状有: *腹痛(最后局限于右下腹) *高热 *食欲减退 *恶心呕吐 医生会对你作如下检查: *腹部检查,可发现腹壁紧张 *肛门指检,可发现阑尾增大 *血液检查,可发现白细胞增高 *对于女性病人还要进行盆腔检查,排除由于卵巢或子

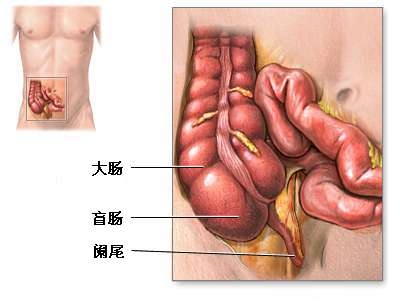
阑尾是细长的条索状肠组织,位于盲肠与回肠之间。

当发生急性阑尾炎时,必需施行紧急阑尾切除术,避免阑尾穿孔导致全腹感染(腹膜炎)。
急性阑尾炎的症状有:
*腹痛(最后局限于右下腹)
*高热
*食欲减退
*恶心呕吐
医生会对你作如下检查:
*腹部检查,可发现腹壁紧张
*肛门指检,可发现阑尾增大
*血液检查,可发现白细胞增高
*对于女性病人还要进行盆腔检查,排除由于卵巢或子宫疾病引起的腹痛。
至今,仍没有确切的检查方法来确诊阑尾炎,实际上,某些症状是由其他疾病原因引起的。医生只能从病人的病史、检查结果来作出诊断。在阑尾切除手术中,有25%的病人会被发现并没有阑尾炎,此时,外科医生检查过腹部其他脏器后,会切除正常的阑尾,以免病人日后发生阑尾炎。

手术切口位于病人的右下腹。

对病人施行常规麻醉后开始手术。术中若发现阑尾有脓肿或阑尾已经穿孔,则要对全腹进行清洗。感染严重者术后还要留置引流管。
极少情况下,阑尾切除术也会用腹腔镜来进行。这通常是用在有不确定的腹痛的女性病人身上。

单纯阑尾切除术术后病人恢复很快,大部分病人术后三天可以出院,一到两周内就可以恢复正常饮食。如果是阑尾脓肿或阑尾穿孔的病人,术后恢复比较慢,而且需要用抗生素来控制感染。阑尾切除后对病人的健康不会造成影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
33
#正常解剖#
31
#手术切口#
41
有文有图
111
好文章,值得收藏
91
#适应症#
14