伴颈椎过伸的强直性脊柱炎脊柱后凸畸形1例
2019-12-27 郑国权 王天昊 宋迪煜 中国脊柱脊髓杂志
强直性脊柱炎(AS)主要累及中轴骨及关节,常从骶髂关节向头侧逐渐进展,晚期常易出现胸腰段后凸畸形。部分AS患者常常累及整个脊柱的强直,包括颈椎、胸椎、腰椎的强直,严重影响患者生活质量。颈椎畸形多为颈椎后凸畸形,如颌-胸畸形,而颈椎过伸畸形相对较为少见,畸形不严重者多无需外科干预。我们在临床中可以遇到某些极特殊的病例,胸腰段后凸畸形很大,但颌眉角(CBVA)增大幅度不大,甚至仍然在正常范围。究其原因
强直性脊柱炎(AS)主要累及中轴骨及关节,常从骶髂关节向头侧逐渐进展,晚期常易出现胸腰段后凸畸形。部分AS患者常常累及整个脊柱的强直,包括颈椎、胸椎、腰椎的强直,严重影响患者生活质量。颈椎畸形多为颈椎后凸畸形,如颌-胸畸形,而颈椎过伸畸形相对较为少见,畸形不严重者多无需外科干预。我们在临床中可以遇到某些极特殊的病例,胸腰段后凸畸形很大,但颌眉角(CBVA)增大幅度不大,甚至仍然在正常范围。究其原因在于人是直立动物,当存在严重胸腰段后凸畸形时,需要伸髋或屈膝(关节未融合)以获得相对的平视功能,而极少数人则通过过渡抬头,即颈椎过伸来获取平视功能。此类患者,矫正胸腰段后凸畸形必然会减小CBVA角度,甚至成为负值。由于颈椎已经强直融合,胸腰段矫正后颈椎过伸畸形带来的新的系列不适将表现出来。这对截骨矫形设计提出了新的困难,整体治疗中有必须考虑通过颈椎的屈曲截骨以纠正过伸畸形。然而,目前文献中对此类病例报道较少,且处理策略缺少共识。我院收治1例强直性脊柱炎颈椎过伸畸形的患者,报道如下。
临床资料
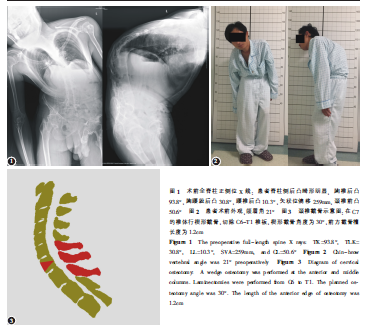
患者男性,36岁。因“脊柱畸形并腰背部疼痛”于2017年10月入院。患者于20年前无明显诱因发现脊柱轻度凸畸形,后症状逐渐加重,腰部疼痛加重,不能平卧。在外院就诊诊断为强直性脊柱炎,患者带药回家治疗,疼痛缓解后停用药物,期间症状反复发作,腰背部疼痛畸形进一步加重,大量活动后出现起得气短,不能正常从事劳力劳动。入院查体:患者站立呈前屈位,脊柱后凸畸形,全脊柱主动、被动活动受限,四肢主动、被动活动自如。辅助检查:全脊柱正侧位X线片上测量,胸椎后凸(TK)93.8°,胸腰段后凸30.8°,腰椎后凸10.3°,矢状位偏移(SVA)259mm(图1)。尽管患者有严重的脊柱后凸畸形并伴有矢状面失平衡,但由于其颈椎前凸(CL)增大为50.6°,CBVA仅为21°(图2),虽然颈椎不能活动,但他仍然能够平视前方,视野能满足日常生活的需要。但由于不能平卧和正常直立,要求手术改善畸形提高生活质量的要求较为强烈。
手术设计因此与患者及家属沟通后,拟一期行胸腰椎后凸畸形矫形,二期行颈椎过伸畸形矫形。其中一期采用双节段VCD的不对称截骨方式部分矫正胸腰椎的后凸畸形,同时纠正冠状面失衡。于2017年10月16日在全麻下行脊柱后路截骨矫形、椎弓根钉棒系统内固定术。六个月后,患者于2018年4月25日行颈椎前后路联合截骨、后路椎弓根钉棒系统内固定、前路钛板螺钉内固定手术。
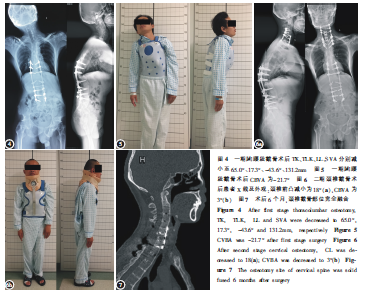
颈椎截骨手术技术(图3):麻醉成功后,患者取仰卧位,身下铺塑形垫,项部及枕下垫枕并固定,常规消毒铺无菌巾,取颈前左侧斜切口,依次切开皮肤、皮下组织及颈阔肌,沿胸锁乳突肌与内侧带状肌的间隙向内分离,经颈动脉鞘内侧达椎前筋膜,切开椎前筋膜,显露C6、C7椎体前方,透视下确认C6/7椎间隙,自动牵开器向两侧及头尾方向牵开周围组织,先在C7椎体前方行楔形截骨,超声骨刀去除椎体内的松质骨,直到颈椎后纵韧带前方,用流体明胶和明胶海绵填塞截骨槽止血,用纱布将截骨椎与前方食管隔离保护,填塞并简单缝合包扎伤口,无菌塑料贴膜保护前方切口,无菌敷料。然后头架固定头部,取俯卧位,颈后正中切口,切开皮肤、皮下组织及筋膜用电刀切开项韧带,沿项韧带向深部分离至棘突、向两侧骨膜下剥离附着在棘突、椎板上的肌肉,自动牵开器向两侧牵开切口显露颈椎后方结构,于C4、C5、C6及T2、T3、T4两侧椎弓根置入椎弓根螺钉,透视见椎弓根螺钉位置佳,用咬骨钳、椎板咬钳及超声骨刀去除C6、C7,和部分T1椎板及C7两侧关节突和椎弓根。充分显露C7、C8神经根,探查并扩大神经根管,在C5、T2行椎板潜行减压,确保神经无压迫。截取合适长度的矫形钛棒,预弯后置入右侧胸螺钉凹槽、拧入螺母,通过降低头架闭合前方截骨间隙,复位颈椎,同时轻微向左侧偏,以纠正冠状位失衡。复位过程中观察硬膜,至硬膜有拉伸,即可停止屈曲操作。拧紧螺帽固定。透视见颈椎畸形纠正,矢状面及冠状面平衡良好。锁紧固定螺母,同时用冰盐水冲洗保证术野脊髓低温。术中透视见内固定位置良好,彻底冲洗切口去除患者头架,再次翻身患者取仰卧位,常规消毒铺无菌巾。再次经颈前切口依次进术区,自动牵开器向两例及头尾方向牵开周围组织,探查见C7椎体截骨面完全闭合,进一步行钛板固定,于C6、C7、T1、T2椎体各置入螺钉两枚。术中透视见内固定位置良好,彻底冲洗切口,清点器械敷料无误,检查无活动性出血,逐层缝合切口。无菌敷料包扎,颈托外固定。
结果手术过程顺利,术中出血约1300ml,输AB型异体红细胞6U,普通冰冻血浆5.6U。术中全程脊髓电生理监测,SEP及MEP无明显变化。患者术后清醒,病情稳定,四肢感觉及运动功能正常。术后3d患者佩戴颈托下地活动。第一次术后TK、TLK、腰椎前凸(LL)、SVA分别减小至65.0°、17.3°、-43.6°、131.2mm(图3)。由于颈椎完全融合,术后CBVA为-21.7°(图4)。术后6个月随访,复查X线及CT见颈椎截骨部位已融合(图5)。此时患者虽然恢复了矢状面平衡,但无法平视,影响生活质量。第二次术后患者CBVA为2.9°(图6)。
讨论
强直性脊柱炎的截骨策略有多种设计方法。整体术前设计:Song等以及Zheng等提出基于肺门法的个性化截骨设计方法,根据患者的骨盆参数计算截骨角度,恢复矢状位平衡。重建矢状面平衡和恢复患者平视能力是矫正脊柱后凸畸形手术的最主要的目的。对于颈椎强直的患者来说,术后视野必须考虑到手术设计当中。在极少数强直性脊柱炎患者,随着脊柱的后凸加大,患者会通过颈椎过伸来维持水平视野。在对此类患者的截骨矫形时,仅考虑矢状面平衡进行矫形,则可能使患者在术后视野朝上,无法平视和低头,从而影响生活质量。因此,在矫正颈椎强直的AS脊柱后凸时,通常会在保持功能视野和矫正矢状面平衡中做出妥协,牺牲后者以保证患者术后能平视前方,通过减小截骨角度来保证视野。
颈椎截骨难度高,并且存在着较大的神经血管损伤风险。在既往报道中,大部分病例是颈椎后凸或屈曲畸形,通常采用单纯后路在C7或T1椎体进行楔形后伸截骨,用以矫正颈段或颈胸段的后凸畸形。以往报道中,通常是通过单纯后路在C7或T1椎体进行楔形截骨矫正颈胸段的后凸。而在此病例中,由于患者颈椎前凸较大,为过伸畸形,因此需要通过颈椎的屈曲截骨减小颈椎前凸,使患者恢复平视能力。颈椎后凸畸形截骨矫形技术已相对成熟,而对颈椎过伸截骨的报道则相对较少。检索相关英文文献数据库,共报道4例患者,笔者将其总结如下。
Sengupta等在侧卧位下行颈椎后前路联合截骨减小患者颈椎前凸。在该例报道中,首先经颈椎后路横形切除C7椎板并显露C8神经根;再在同一体位下,经颈椎左前方斜切口显露C7椎体并行楔形截骨,随后辅助哈罗氏架行颈椎屈曲闭合,再用颈椎前路钉板固定。此颈椎屈曲截骨为后方张开、前方闭合。此外,闭合过程中存在椎体后壁的骨折,这也有一定的脊髓损伤风险。Kose等报道了3例Becker型肌营养不良导致的颈椎过伸畸形的病例。他们采用前-后-前的入路,首先是仰卧位行前路手术,选择以C7/T1椎间盘为中心的楔形截骨,切除C7/T1椎间盘及上下部分椎体,然后俯卧位行后路松解手术,切除C7、T1棘上、棘间韧带,侧块或椎弓根螺钉固定,在脊髓监测下,由台下助手将头颈部屈曲固定,可见C7、T1棘突间明显张开;最后仰卧位行前路钛板螺钉固定。此截骨同样存在脊髓被延长的风险,由于后方椎板未切除,无法直视监控矫形过程中脊髓的状态,而且Kose的方法适用于后方结构没有骨性融合的病例,因此不适合强直性脊柱炎患者的颈椎截骨。如果要采用Kose的方法处理颈椎后方有骨性融合的病例,需在此基础上增加后方骨性结构的切除、神经减压。在本文报道病例中,由于患者术前胸腰段后凸畸形严重,而CBVA基本正常,如按Zheng等提出的双节段截骨设计,我们选择在T12、L2(靠近后凸顶点,且相对安全)行双节段截骨,在不考虑颌眉角的情况下需要的截骨角度为:T12=50°,L2=60°,这虽然恢复了患者的矢状面平衡,但术后患者会抬头望天,失去水平视野。若考虑颌眉角而减小矫正率,按照最佳CBVA计算截骨角度,那么其大小不应超过CBVA+(PT-tPT)=49°,这虽然保证了患者的水平视野,但矫正不足导致术后仍然严重失平衡。因此采用分期手术策略是非常必要的:一期行胸腰段截骨,恢复矢状面平衡;二期颈椎截骨,恢复水平视野。
单纯后路经C7去松质骨楔形闭合截骨能够完成对颈椎或颈胸后凸畸形的矫形,但对于颈椎过伸畸形,需要屈曲截骨,如果单纯采用前路或后路均不能完成。单纯后路截骨难以短缩前柱,减小前凸,且无法保护脊柱前方软组织,如食道等。而通过后柱延长会增加神经损伤的风险。单纯前路手术虽然能短缩前柱及中柱,但在由于后柱已经融合,这使复位过程难以完成。如果采用后-前或后-前-后的入路,那么在前路进行复位、闭合时无法监控脊髓的状态,使脊髓损伤风险增加。因此,在此病例中,我们并没有文献报道的后-前或后-前-后入路,而是采用前-后-前联合入路进行颈椎屈曲截骨矫形。第一步前路手术在C7椎体行楔形截骨,且截骨面对应椎弓根,实际上截除的骨面更类似于梯形,相当于楔形的顶点位于椎弓根中点或者说是脊髓平面,同时,由于该患者颈椎完全融合,即使在前柱截骨后,后方结构仍然维持了颈椎的稳定性,保证了体位变换过程中的安全。此外,首先进行前路截骨可以用纱布把食道和截骨椎隔离开,降低食道损伤风险。第二步后路手术完成后方椎板减压、经C7椎弓根截骨和复位过程。经C7椎弓根截骨一方面可以延续前方的楔形截,另一方面通过C7截骨可以使脊髓腹侧、背侧空间相通,避免椎体骨折或去除其他潜在损伤脊髓的骨质。此外,整个复位过程中脊髓始终在直视下,可以一定程度上避免神经损伤的发生,而且在后路术者可以根据脊髓状态控制矫形的程度及进程。第三步再行前路钛板螺钉固定手术不仅可以增加强直性脊柱炎患者颈椎稳定性,而且可以验证前方截骨面闭合情况,观察有无食道损伤情况。
术中操作要点及注意事项:(1)先前路操作过程中注意保护食道,为了避免矫形过程中、椎体前方闭合时损伤食道等脏器,可于C7椎体楔形截骨处用面胶海绵填塞,同时纱布临时隔离食道;(2)C7椎体前方的楔形截骨时注意暂且保留后纵韧带,降低椎管内的静脉丛出血风险,影响手术进程;(3)后路手术时后方的减压一定要充分,尤其是对C7、8神经根的松解、减压;(4)复位过程中注意台上、台下的密切配合,控制头架活动与台上的操作要一致,幅度切忌不可过大;(5)后路屈曲矫形过程中观察到硬膜有拉伸,即可停止屈曲操作。
综上所述,我们认为前-后-前联合入路、经C7屈曲截骨能够顺利纠正强直性脊柱炎患者的颈椎过伸畸形,术前的精准截骨设计、术中的精细操作对手术的成功必不可少。当然,颈椎过伸畸形病例较为少见,此术式的安全性、有效性仍有待于进一步临床验证。
原始出处:
郑国权,王天昊,宋迪煜,王征,王岩.伴颈椎过伸的强直性脊柱炎脊柱后凸畸形1例报道[J].中国脊柱脊髓杂志,2019,29(10):940-943.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#颈椎过伸#
63
#强直性#
32
#后凸畸形#
39
#畸形#
48
#脊柱炎#
45