【一般资料】
患者,43岁
【主诉】
因卵巢颗粒细胞瘤术后2年,发现盆底多发结节3周,于2016年5月6日入我院。
【现病史】
【既往史】
患者既往月经规则,经期7天,周期27~30天,经量中等。
【月经及婚育史】
G0P0。
【治疗】
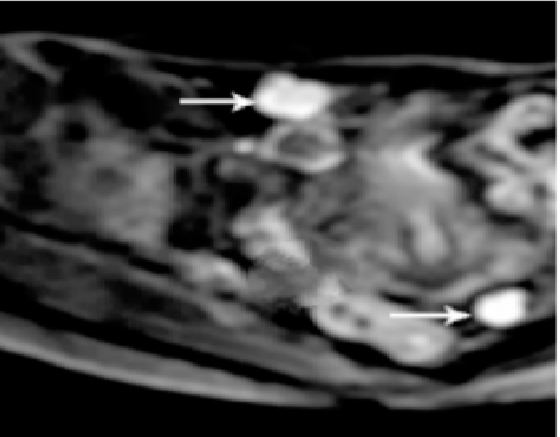
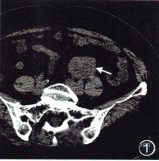
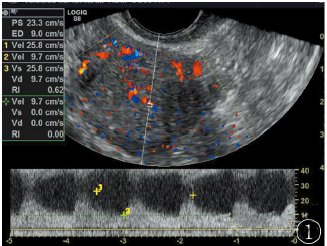
2014年6月12日因右侧附件区囊性占位(45mm×49mm×53mm)于我院行腹腔镜下右侧卵巢囊肿剥除术+缝合修补成形术。术中见右侧卵巢一直径6cm大小囊肿,表面光滑,未见明显包膜,内含脂肪样组织,血运不丰富。右侧输卵管及左侧附件未见明显异常。子宫前位,正常大小,外观未见明显异常,无腹水。术后病理检查示:右侧卵巢肿瘤细胞角蛋白(CK)(-),上皮膜抗原(EMA)(-),抑制素(inhibin)(+),波形蛋白(VIM)(+),钙视网膜蛋白(calretinin)(+),CD99(+),CD117(-),结合HE切片,符合右侧卵巢颗粒细胞瘤(成年型)。患者于2014年7月9日再次行腹腔镜下右侧附件切除术+大网膜切除术+腹膜活检术,术中子宫、右侧输卵管、左侧附件区如前次所见,右侧残余卵巢表面光滑,与阔韧带后叶膜状粘连,呈术后改变。探查盆腹腔、腹膜、大网膜、阑尾、肝、脾、膈无明显转移结节,腹水少量。术后病理检查示:“右侧卵巢”可见颗粒细胞瘤组织残余,最大直径1.5cm,伴坏死囊性变。“右侧输卵管”、“大网膜”、“左、右侧结肠旁沟腹膜”均未见肿瘤细胞。患者术后诊断成人型卵巢颗粒细胞瘤IC期,于2014年7月26日行第1次静脉化疗,方案为紫杉醇联合卡铂。后因个人原因未再行化疗,于门诊定期随访。2014年8月至2015年11月门诊随访期间均无异常发现。2016年1月13日行盆腔CT平扫+增强扫描结果示:盆底偏左侧结节12mm;4月15日再次复查CT提示:盆底多发软组织结节灶,最大18mm,考虑转移瘤(图1A、1B);4月14日行盆腔MRI增强+弥散加权成像(DWI)检查示:盆底多发软组织结节灶,考虑转移瘤,与2016年1月13日CT片比较,左侧盆底结节略增大,近右侧腹股沟管内口可见新发结节(图1C、D)。考虑该患者卵巢颗粒细胞瘤复发拟行手术,术前为评估是否存在远处转移,故于4月22日行正电子发射计算机断层显像(PET-CT)检查,结果提示:左侧盆底可疑结节,结节氟化脱氧葡萄糖(FDG)代谢未见明显增高,肝右叶低密度灶,右肾结石及小囊肿(图2)。患者于2016年5月9日行腹腔镜探查,术中见右侧腹前壁结节约1.0cm×1.5cm,质地中等;左侧结肠系膜粘附于侧盆壁,见多个散在结节,较大两个约3cm×2cm大小;左侧盆壁、右侧盆壁、直肠表面及结肠带见多发结节,直径约0.5~1.5cm。盆腔无明显腹水,子宫正常大小,无特殊改变,右侧附件缺如,左侧附件区见2枚1cm×1cm囊肿。遂行全子宫+左侧附件切除术+盆腔淋巴结切除术,术后病理检查示:“左盆壁结节”“右盆壁结节”“直肠表面结节”“盆底结节”“结肠带结节”“右侧腹壁结节”均见颗粒细胞瘤浸润(图3A),“左附件区结节”系膜囊肿,“全子宫”子宫内膜增生反应,宫颈慢性炎,宫体浆膜下结节见肿瘤组织浸润,左附件、阴道切缘、“左盆腔淋巴结(0/5)”、“盆腔淋巴结(0/6)”均未见肿瘤细胞。免疫组化示:“左盆壁结节”肿瘤细胞,S-100蛋白(+),钙视网膜蛋白(calretinin)(-),CD99(+),α-inhibin(-),ER(+),PR(+),ki-67(<10%)(+)(图3B),嗜铬素A(CgA)(-),突触素(SYN)(-),CD56(+)。术后1周患者行BEP方案静脉化疗,目前尚在治疗中。
【讨论】
2.1卵巢颗粒细胞瘤复发的CT及MRI诊断卵巢颗粒细胞瘤属于性索间质肿瘤,是一种相对罕见的低度恶性肿瘤,约占所有卵巢恶性肿瘤的2%~5%,预后一般较好,5年无瘤生存率(DFS)和总生存率(OS)在72%~99%。颗粒细胞瘤有晚期复发或转移倾向,复发率为21%,平均复发时间为57.6个月(2~166个月),复发转移后预后较差。多数复发病灶位于盆腹腔,常发生在与原发灶有联系的部位。由于卵巢颗粒细胞瘤复发时常见的肿瘤指标如CA125、CA199及CEA往往在正常范围,因此影像学检查在诊断颗粒细胞瘤复发中的作用显得尤为重要,但目前这方面的资料较有限。姬妮娜等描述卵巢颗粒细胞瘤原发病灶多表现为单侧附件区边界清楚的类圆形、分叶状肿块,可以呈囊实性、实性及囊性表现,以囊实性最为常见,肿块内可见多发大小不等的囊状或片状低密度,囊壁及分隔厚薄不一,但无壁结节;CT增强扫描实性部分可呈轻、中度或明显强化,强化程度低于子宫肌层;可伴腹水,但一般无淋巴结肿大。他们的病例中包括两例卵巢颗粒细胞瘤复发患者,CT表现盆腹腔散在肿块,与原发肿瘤相似呈囊实性蜂窝状。Rha等描述了11例复发性卵巢颗粒细胞瘤患者的CT及MRI,病灶可表现为单房囊性肿块、囊实性肿块,亦可表现为实性肿块,MRI还提示出血为复发性颗粒细胞瘤的非特性特点之一。Kim等描述中有2例复发性卵巢颗粒细胞瘤患者,CT及MRI影像学表现为伴不同程度囊变区的实性肿块和多分隔的囊性肿块。本例患者CT及MRI检查示盆底多发软组织结节,为边界清楚的类圆形、实性肿块,CT增强部分呈轻中度强化(图1A、B),MRI增强后明显强化(图1C、D),这与已有文献报道类似。DWI是目前唯一能够观察活体组织内水分子弥散的一种无创性检查技术,它从细胞或分子水平描述肿瘤内部微观结构的变化,提供肿瘤细胞密度、细胞膜完整性的组织病理学信息。病理状态下,细胞内外的大分子分布改变及膜结构的完整性遭到破坏,组织水分子弥散受限程度改变而使DWI信号表现异常。肿瘤组织细胞较其组织起源细胞更加紧密,密度构成增大,细胞内部结构密度也增大,均可造成肿瘤内水分子弥散受限,DWI信号相对升高。本例患者MRI+DWI检查中发现病灶处水分子弥散受限,表现为DWI明显高信号(图1D),高度提示肿瘤复发可能。2.2卵巢颗粒细胞瘤复发的PET-CT表现目前最常用的PET显像剂为18F标记的FDG(18F-FDG),是一种葡萄糖的类似物。恶性肿瘤细胞由于代谢旺盛,导致对葡萄糖的需求增加,因此静脉注射18F-FDG后,大多数肿瘤病灶会表现为对18F-FDG的高摄取,因此PET-CT显像可早期发现肿瘤原发及转移病灶,准确判断其良、恶性,从而指导临床治疗。本例患者因拟行手术,术前为评估是否存在远处转移故行PET-CT检查,然而PET-CT的结果出乎意料,即CT见左侧盆底可疑结节,但结节FDG代谢未见明显增高(见图2)。迄今有关PETCT诊断卵巢颗粒细胞瘤复发的研究极少,仅见于零星个案报道,因此其诊断价值尚不明确。Caoduro等报道了1例颗粒细胞瘤术后复发转移,转移灶最初位于右侧髂骨,后肿瘤转移至肺部、髂骨其他部位,PETCT均显示强阳性。Huang报道的颗粒细胞瘤术后复发转移病例中,患者行PET-CT检查,复发灶FDG代谢增高,然而转移灶中FDG代谢呈现高低不均的趋势。Miyazaki等个案中报道了1例颗粒细胞瘤腹腔镜手术后盆腔原患侧卵巢处复发,PET-CT提示复发灶阳性结节。然而也有一些个案报道与本文类似,最终确诊的颗粒细胞瘤复发病灶行PET-CT为假阴性结果。Günyeli等2014年报道1例原发性卵巢颗粒细胞瘤合并子宫内膜癌患者PET-CT结果表现为卵巢颗粒细胞瘤18FFDG低摄取。Raj等个案报道中描述了2例卵巢颗粒细胞瘤复发患者行PET-CT检查假阴性,均于CT检查中发现复发病灶,而病灶18F-FDG呈低摄取。此外Kimura等报道1例卵巢颗粒细胞瘤患者发生肺部转移,行PET-CT检查,但复发转移结节中无FDG摄取。为何卵巢颗粒细胞瘤病灶会呈现18F-FDG低或无摄取?我们推测这与颗粒细胞瘤增殖水平较低有关。ki-67抗原为细胞核内与细胞分裂增殖相关的蛋白抗原,是一个反映细胞增殖的敏感指标。在卵巢癌中ki-67表达水平与18F-FDG摄取呈显著正相关。已有研究报道卵巢交界性肿瘤行PET-CT检查亦会出现高比例的假阴性结果,与卵巢恶性肿瘤相比,卵巢交界性肿瘤的代谢及增殖活性显著降低,这体现在卵巢交界性肿瘤的增殖细胞核抗原ki-67染色呈现弱阳性。本例患者复发的肿瘤细胞中ki-67染色阳性率<10%,提示肿瘤细胞增殖指数在较低水平(图3A),推测18F-FDG摄取少,故PET-CT为假阴性结果。PET-CT目前已在临床广泛应用,对于评估恶性肿瘤治疗效果及监测肿瘤复发具有极其重要的意义,但对于细胞增殖水平低的某些特殊类型肿瘤可能存在假阴性结果。本例个案报道提示临床工作者利用PET-CT评估卵巢颗粒细胞瘤复发时,对于阴性结果需要持有审慎的态度,需结合CT或MRT+DWI综合判断。

1A CT 增强横断截面图像
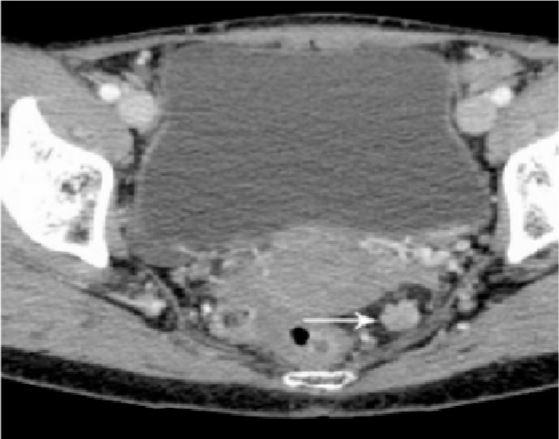
1B CT 增强横断截面图像
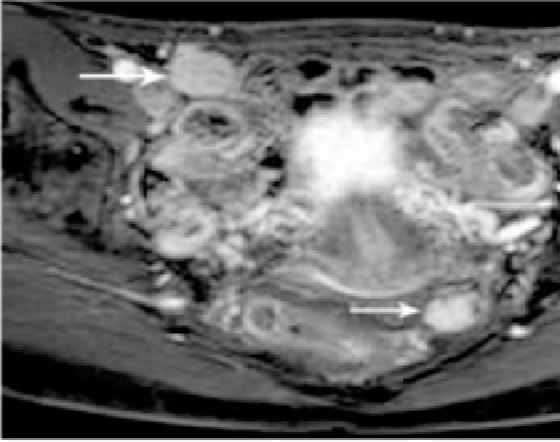
1C 增强盆腔 MRI 图像
1D MRI 弥散加权成像( 箭头所示为颗粒细胞瘤复发灶)

图 1 CT 及 MRI 检查图像

图 2 PET-CT 假阴性结果,颗粒细胞瘤复发灶 FDG 代谢未见明显增高
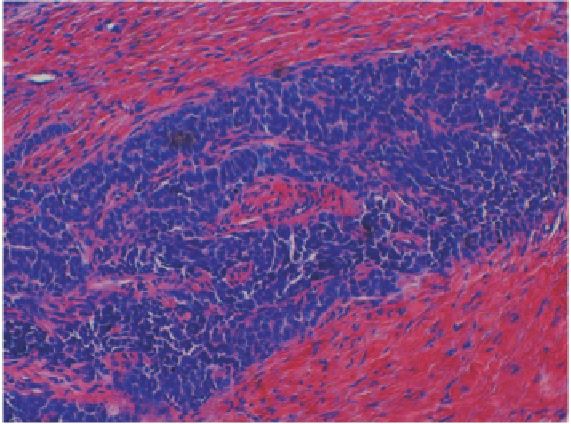
3A 肿瘤细胞呈多边形,大小较一致,核大而深染,胞 质空泡,符合成人型颗粒细胞瘤 ( HE×20)

3B ki-67( <10%) ( +) ( 免疫组化×20)图 3 病理检查及免疫组化 ki-67 检测图
原始出处:
熊云棋, 吴霞. 卵巢颗粒细胞瘤复发PET-CT检查假阴性1例[J]. 实用妇产科杂志, 2017, 33(1):74-76.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
34
#PET#
0
#细胞瘤#
31
#颗粒细胞瘤#
32
谢谢分享学习
59