Lung Cancer:亚洲人群分析!PD-L1高表达提示EGFR突变肺腺癌对EGFR-TKI的原发耐药!
2019-02-11 肿瘤资讯 肿瘤资讯
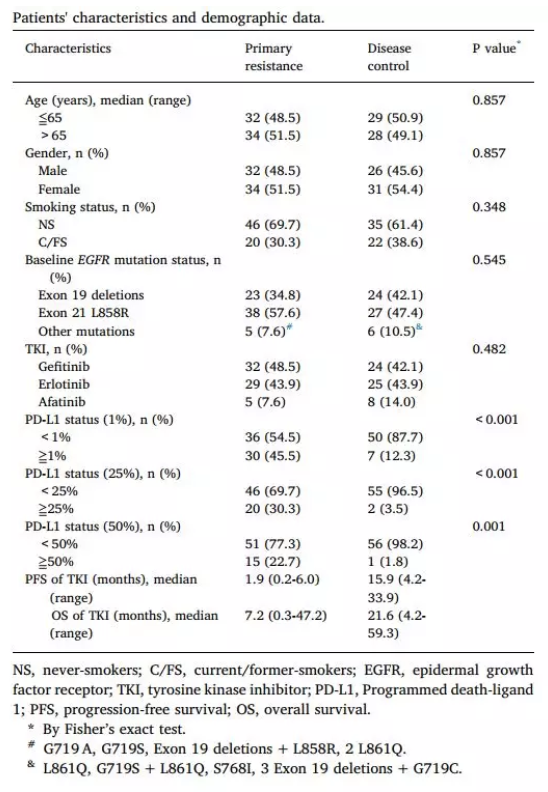
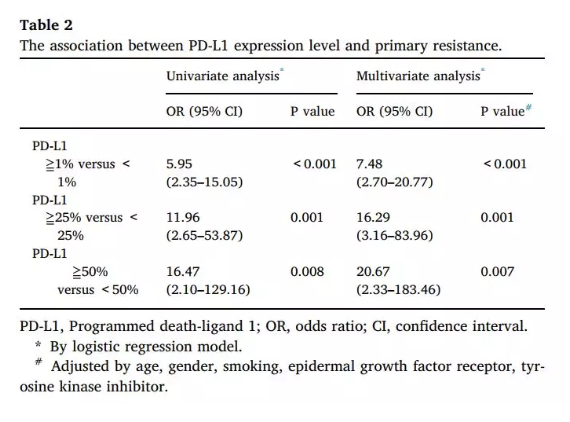
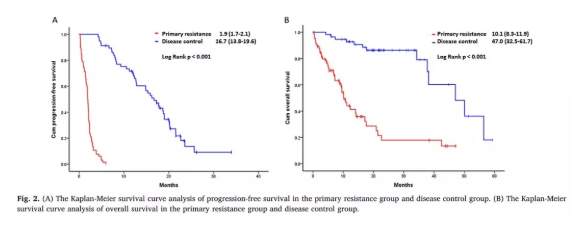
与含铂化疗相比,表皮生长因子受体酪氨酸激酶抑制剂(EGFR-TKI)在非小细胞肺癌(NSCLC)的治疗中显示更好的应答率和较少的不良反应。但是5%~10%的敏感EGFR突变患者对EGFR-TKI治疗会产生原发性耐药,目前耐药机制尚不清楚。近日,一项来自中国台湾的回顾性研究评估了对EGFR-TKI治疗产生原发耐药的EGFR突变肺腺癌患者的PD-L1表达水平,研究结果刊登在Lung Cancer杂志上


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PD-L1#
42
#EGFR-TKI#
26
#TKI#
37
#GFR#
29
#亚洲人群#
52