Lancet oncol:激素疗法的顺序和放射照射的面积对前列腺癌患者预后的影响
2018-10-13 MedSci MedSci原创
NRG/RTOG 9413研究显示,与仅对前列腺进行放射治疗(PORT)联合新辅助激素治疗(NHT)、全骨盆放疗(WPRT)联合辅助激素治疗(AHT)和PORT联合AHT相比,WPRT联合NHT可提高中高风险的局限性前列腺癌患者的无进展存活率。现Prof Mack Roach等人对激素疗法的顺序和放射照射的面积对前列腺癌患者预后的影响进行研究。研究人员设计了一个2x2的阶乘研究,以激素治疗顺序和放
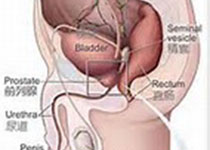
研究人员设计了一个2x2的阶乘研究,以激素治疗顺序和放射区域为分层因素,验证NHT相比AHT、NHT+WPRT、NHT+PORT,是否可提高前列腺癌患者的无进展存活率。招募病理确诊的局限性的前列腺腺癌患者,并要求淋巴结转移风险>15%、Karnofsky表现状态>70,无年龄限制。将受试患者随机(1:1:1:1)分至NHT+WPRT组(WPRT治疗前和治疗中各予以NHT2治疗2个月,膀胱放射量70Gy)、NHT+PORT组(PORT前和中NHT治疗2个月,放射量70Gy)、WPRT+AHT组(WPRT治疗后AHT治疗4个月)和PORT+AHT组(PORT后AHT治疗4个月)。激素疗法结合雄激素抑制,包括醋酸戈瑞林 3.6mg/月 皮下注射 或醋酸亮丙瑞林 7.5 mg/月 肌注、氟他胺250mg/天 口服 4个月。并根据T分期、Gleason评分和前列腺特异性抗原浓度进行分期。NHT治疗在放疗前2个月开始,并持续至放疗结束;AHT治疗在放疗结束后开始,持续4个月。主要结点:无进展存活率。
1995年4月1日-1999年6月1日,共从53个国家招募了1322位患者,患者被随机分至4个治疗组。对于所有患者的中位随访时间为8.8年(IQR 5.07-13.84),对于存活患者(346位)随访时间为14.8年(7.18-17.4),在4个治疗组中,所有时间节点的无进展存活率均存在显著差异(p=0.002)。NHT+WPRT组、NHT+PORT组、WPRT+AHT组和PORT+AHT组的10年无进展存活率分别是28.4%(95% CI 23.3-33.6)、23.5%(18.7-28.3)、19.4%(14.9-24.0)和30.2%(25.0-35.4)。膀胱毒性是最常见的3级(或更严重)晚期毒性,NHT+WPRT组、NHT+PORT组、WPRT+AHT组和PORT+AHT组的发生率分别为6%(18/316)、5%(17/313)、7%(22/317)和4%(14/316);3级及以上胃肠道副反应的发生率分别是7%、2%、3%和2%。
在中高风险的局限性前列腺癌患者队列中,相比NHT+PORT和WPRT+AHT疗法,NHT+WPRT疗法可显著提高患者的无进展存活率,虽然会增加3级及以上的肠道毒性风险。放疗和激素治疗的相互作用提示WPRT应与NHT配合使用。
Prof Mack Roach,et al. Sequence of hormonal therapy and radiotherapy field size in unfavourable, localised prostate cancer (NRG/RTOG 9413): long-term results of a randomised, phase 3 trial. The Lancet Oncology. October 10,2018.https://doi.org/10.1016/S1470-2045(18)30528-X
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者预后#
31
#Oncol#
32
#Lancet#
27
学习了
76
?
72
#激素疗法#
35
好
68
学习了
55
了解一下谢谢
64
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
26